
Abdul Mannan: BDUC – 4 Letters That Make Many Haematologists Uncomfortable
Abdul Mannan, Consultant Haematologist at Betsi Cadwaladr University Health Board, shared on LinkedIn:
”BDUC. Four letters that make many haematologists uncomfortable.
Bleeding Disorder of Unknown Cause. The patient bleeds. Your tests are normal.
Now what?
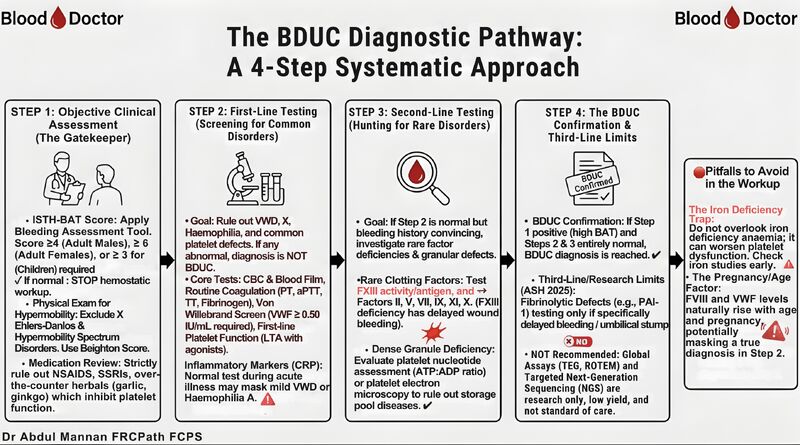
I’ve developed a 4-step systematic approach to navigate this clinical challenge:
Step 1: The Gatekeeper
Apply ISTH-BAT Score (≥4 men, ≥6 women, ≥3 children)
If normal, stop. No hemostatic workup needed.
Check for hypermobility syndromes and medication culprits (NSAIDs, SSRIs, garlic, ginkgo)
Step 2: Rule Out Common Disorders
CBC, blood film, routine coagulation, VWF screen (≥0.50 IU/mL required)
First-line platelet function (LTA with agonists)
Remember: Inflammation masks mild VWD and Haemophilia A
Step 3: Hunt for Rare Disorders
If Step 2 is normal but bleeding history is convincing, test FXIII (delayed wound healing!) and Factors II, V, VII, IX, XI, X
Consider dense granule deficiency with ATP:ADP ratio or electron microscopy
Step 4: Confirm BDUC
High BAT score + completely normal Steps 2 and 3 equals BDUC confirmed
Test fibrinolytic defects only if delayed bleeding or umbilical stump issues (ASH 2025)
TEG, ROTEM, NGS? Not standard of care. Low yield.
Two pitfalls I see repeatedly: Overlooking iron deficiency (worsens platelet function)
Testing FVIII/VWF during pregnancy or inflammation (falsely normal)
The visual flowchart is in the comments below.
What’s your approach when bleeding history is strong but labs are normal?”
Stay updated with Hemostasis Today.
-
Jan 26, 2026, 05:40Vicki Kopplin Offers Immediate Funding for People With Bleeding Disorders
-
Jan 26, 2026, 05:27Jill Storry on Alloimmune Hemolytic Disease of the Fetus And Newborn
-
Jan 26, 2026, 05:09Wathsala Manindrani Gives a A Practical Perspective on Red Cell Exchange Transfusion
-
Jan 26, 2026, 04:51Manoj Kumar Singh: Power In Me Foundation Celebrates 2026 as Year Of Rare
-
Jan 26, 2026, 04:40Heghine Khachatryan: Did You Know VWD Comprises 3 Main Types?
-
Jan 25, 2026, 15:57Céline Chapelle Shares Clinical Predictors From the API-CAT Trial
-
Jan 25, 2026, 15:42Francesco Lo Monaco on Heart Disease Starting Quiet While Your Labs Speak First
-
Jan 25, 2026, 15:25Muhammad Ibrahim on Efficacy and Safety of Extended DOACs Use in VTE
-
Jan 25, 2026, 15:08Tushar Pandey on Managing Thrombotic Thrombocytopenic Purpura
