
Tareq Abadl on Bacterial Contamination of Platelets
Tareq Abadl, Medical Laboratory Specialist and Director of the Blood Bank at Dr. Abdelkader Al-Mutawakkil Hospital, shared on LinkedIn:
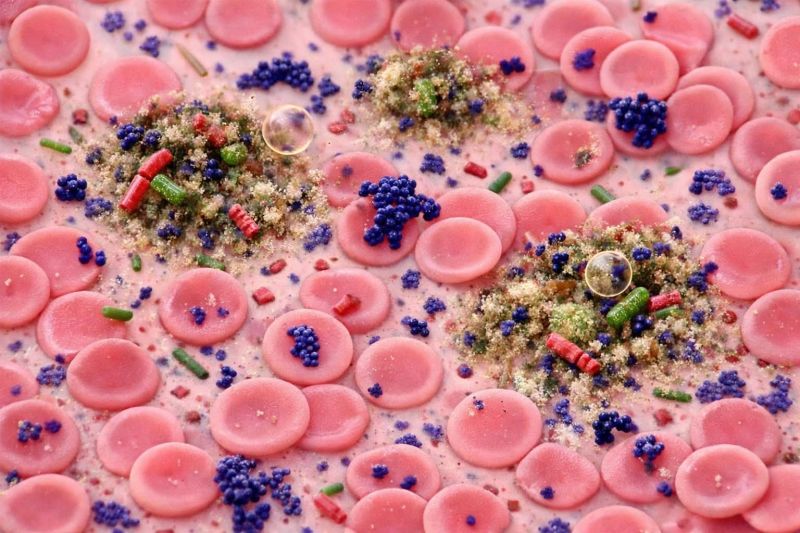
”Bacterial Contamination of Platelets
Why platelets are higher risk
Platelets are stored at room temperature (20–24°C) with agitation, unlike refrigerated components.
This environment favours bacterial growth.
Contamination is uncommon, but when it happens it can cause rapid, severe sepsis.
How common is it?
Detected contamination with standard culture screening: ~1 in 1,000–5,000 units.
Despite the low rate, contaminated platelets cause a disproportionately high share of transfusion-related sepsis and deaths.
Key principle
No single test is 100% sensitive.
Risk reduction depends on a layered strategy, not one method.
Practical Mitigation Strategies
Donor-site controls
Careful skin disinfection
Diversion of the first blood volume
First and most important step to reduce initial contamination.
Primary culture (LVDS – Large-Volume Delayed Sampling)
Improves detection sensitivity before release
Widely used in bacterial-risk control pathways.
Secondary / rapid testing (hospital level)
Can catch contaminated units missed by primary culture
FDA-recognized strategy, especially for day 4–5 platelets.
Pathogen-Reduction Technologies (PRT)
Examples: Amotosalen + UVA, Riboflavin + UV (where approved)
Inactivate many bacteria
Adjunct, not a replacement for cultures, donor controls, or surveillance.
Clinical Red Flags (Think Septic Transfusion Reaction)
Suspect if symptoms occur during or within hours after platelet transfusion:
- Fever
- Chills / rigors
- Hypotension
- Unexplained tachycardia
- Rapid clinical deterioration
Immediate actions
Stop the transfusion
Notify the transfusion service immediately
Follow institutional sepsis and transfusion-reaction protocols.
Operational Checklist (Transfusion Services)
SOPs for:
- Visual inspection
- Storage conditions
- LVDS sampling
- Approved rapid tests
- PRT policy (if used)
Clinical staff training
Early recognition and prompt reporting of reactions.
Hemovigilance
Active surveillance and mandatory reporting
Use local data to balance safety vs supply when choosing between culture, rapid testing, and PRT.
Bottom line
Platelet bacterial contamination is rare but potentially catastrophic.
Safety depends on a layered approach:
donor-site controls + validated culture/testing + secondary rapid testing or PRT + clinician awareness + active hemovigilance.”
Stay updated with Hemostasis Today.
-
Jan 22, 2026, 15:36We Must Roll Up Our Sleeves And Help: José Antonio García Erce on Plasma Donation
-
Jan 22, 2026, 15:25Nita Radhakrishnan on Challenges In Congenital Afibrinogenemia
-
Jan 22, 2026, 15:10Jin Q Gives a Summary of 2025’s Most Impactful Cell and Gene Therapy Milestones
-
Jan 22, 2026, 14:57Nirav Dhanesha on CD14 Acting As A Functional Driver of DVT
-
Jan 22, 2026, 11:41Jamilla Goedegebuur and Colleagues on VTE Management in Case of PAD
-
Jan 22, 2026, 11:28Abdulrahman Katib on API-CAT Trial’s Evaluation of Apixaban Dosing
-
Jan 22, 2026, 11:19Bruno Odisio: Ablation Margins Are Software-Dependent
-
Jan 22, 2026, 10:38Pedro Perez: The VTE Market Is Clearly Entering Its Next Phase
-
Jan 22, 2026, 10:29Marvin Garcia Reyes Presents a Case of Aorto-Visceral and Aorto-Iliac Thrombosis
