
Heghine Khachatryan: Homocysteine – A Small Molecule with Big Clinical Consequences
Heghine Khachatryan, Editor-in-Chief of Hemostasis Today, Head of Hemophilia and Thrombosis Center at Yeolyan Hematology and Oncology Center, shared a post on LinkedIn:
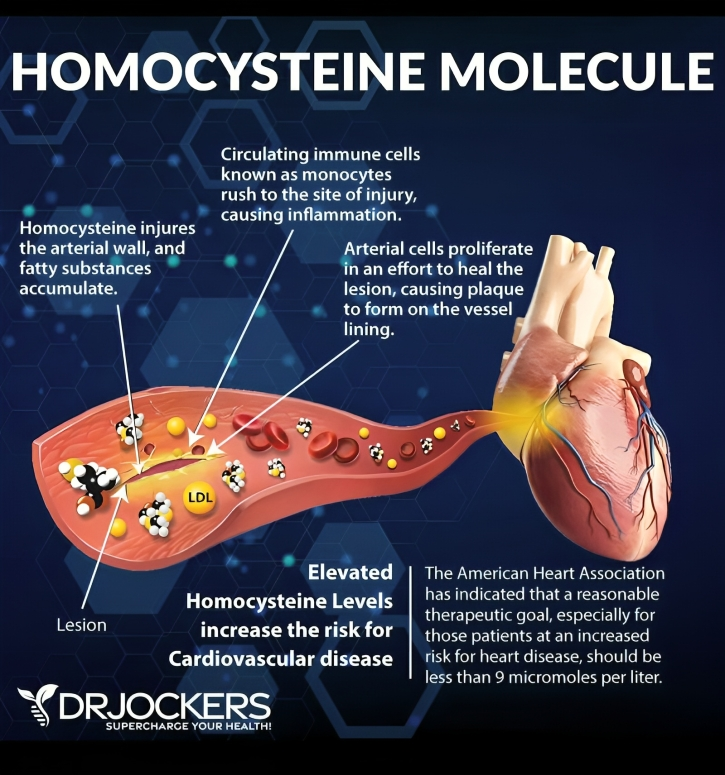
“Homocysteine: a small molecule with big clinical consequences
Homocysteine is an amino acid formed during the metabolism of methionine, which we obtain from protein-rich foods (eggs, meat, fish, cheese, rice, soy, etc.). On its way through metabolic pathways, homocysteine should either be converted to glutathione – our key intracellular antioxidant – or to SAMe (S-adenosylmethionine), a universal methyl donor involved in hundreds of reactions.
Both pathways depend on adequate levels of specific cofactors:
- For homocysteine → glutathione: vitamins B2, B6 and zinc
- For homocysteine → SAMe: vitamins B2, B6, B9, B12, zinc, magnesium and trimethylglycine (TMG, betaine)
When these cofactors are deficient, the reactions slow down, homocysteine accumulates, and we face hyperhomocysteinaemia. In addition to nutritional deficiency, functionally significant variants of the MTHFR gene can impair conversion of folic acid to methylfolate and further disturb homocysteine metabolism.
From a clinical perspective, persistently elevated homocysteine (ideally we aim for <8–9 µmol/L; >20 µmol/L is considered high risk) is associated with:
- Ischaemic stroke
- Alzheimer’s and other dementias
- Parkinson’s disease
- Schizophrenia and other neuropsychiatric disorders
- Atherosclerosis and cardiovascular disease
- Osteoporosis
- Adverse pregnancy outcomes
What can we do in practice?
- Measure homocysteine in appropriate risk groups.
- Assess and correct deficiencies of B-group vitamins, zinc and magnesium (through diet and, when necessary, supplementation).
- Consider the impact of smoking, chronic stress and polypharmacy on micronutrient status.
- In selected cases, evaluate for MTHFR variants and adapt folate therapy (e.g. methylfolate) accordingly.
Homocysteine is a simple marker that sits at the intersection of nutrition, genetics and vascular risk. It deserves more attention both in routine clinical practice and in patient education.”
Stay informed with Hemostasis Today.
-
Jan 25, 2026, 15:57Céline Chapelle Shares Clinical Predictors From the API-CAT Trial
-
Jan 25, 2026, 15:42Francesco Lo Monaco on Heart Disease Starting Quiet While Your Labs Speak First
-
Jan 25, 2026, 15:33Wilfried Dinh: Why Heart Patients Still Have Events Despite ”Optimal” Cardiovascular Therapy
-
Jan 25, 2026, 15:25Muhammad Ibrahim on Efficacy and Safety of Extended DOACs Use in VTE
-
Jan 25, 2026, 15:08Tushar Pandey on Managing Thrombotic Thrombocytopenic Purpura
-
Jan 25, 2026, 14:55Carolina Contreras Cuevas Shares a Nationwide Study on VTE in PAD
-
Jan 25, 2026, 14:40Jeannie Devereaux Links PRP and Physical Therapy
-
Jan 25, 2026, 14:25Heghine Khachatryan on Anticoagulation After AFib Ablation: New Evidence from NEJM
-
Jan 25, 2026, 12:42Lale Tokgözoğlu on Cardiovascular Risk Factors in Women
