
Amy Rivera: Understanding Lymphedema Imaging
Amy Rivera, Founder and Executive Director of the Ninjas Fighting Lymphedema Foundation, shared a post on LinkedIn:
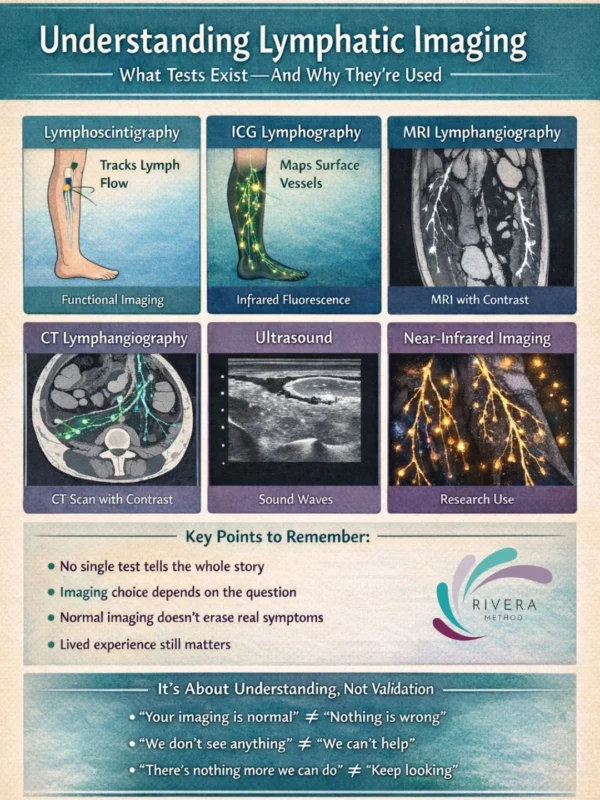
“When lymphedema is suspected, progressing, or not responding as expected, imaging can help answer an important question:
What is actually happening inside the lymphatic system? There isn’t just one imaging option and not every test looks at the same thing.
Lymphoscintigraphy:
What it shows:
- How lymph fluid moves through the body over time.
How it works:
- A small radioactive tracer is injected (usually into the hands or feet), and images track how it travels through lymphatic vessels.
Why it’s used:
- Confirms impaired lymph flow
- Helps diagnose lymphedema
- Often required for insurance or documentation
Limitations:
- It shows function, but not fine structural detail.
Indocyanine Green (ICG) Lymphography:
What it shows:
- Superficial lymphatic vessels and flow patterns just under the skin.
How it works:
- A fluorescent dye is injected and viewed with a near-infrared camera.
Why it’s used:
- Maps lymphatic pathways
- Identifies dermal backflow
- Guides surgical planning
Limitations:
- Only shows superficial lymphatics not deeper structures.
MRI / MR Lymphangiography:
What it shows:
- Soft tissue changes, fluid accumulation, fat deposition, and sometimes lymphatic vessels.
How it works:
- MRI imaging, sometimes with contrast, creates high-resolution images.
Why it’s used:
- Evaluates tissue composition
- Helps differentiate fluid vs fat-dominant swelling
- Useful for surgical planning
Limitations:
- Availability and expertise vary by center.
CT Lymphangiography:
What it shows:
- Anatomical detail of lymphatic structures and surrounding tissues.
How it works:
- CT imaging with contrast.
Why it’s used:
- Specific surgical or anatomical questions
- Less common for routine lymphedema diagnosis
Limitations:
- Radiation exposure; limited functional insight.
Ultrasound:
What it shows:
- Tissue thickness, fibrosis, and fluid characteristics.
How it works:
Sound waves visualize soft tissue.
Why it’s used:
- Evaluates tissue quality
- Monitors changes over time
- Rules out other causes of swelling
Limitations:
- Does not directly visualize lymphatic flow.
Near-Infrared Fluorescence Imaging (Research / Advanced Centers):
What it shows:
- Dynamic lymphatic flow and vessel function.
Why it’s used:
- Research settings
- Specialized surgical centers
- Advanced diagnostic insight”
Stay updated with Hemostasis Today.
-
Feb 13, 2026, 13:53What if Hemophilic Joint Damage Isn’t as Irreversible as We Thought? – RPTH Journal
-
Feb 13, 2026, 13:52Wolfgang Miesbach: Adding Years of Life – and Life to Years
-
Feb 13, 2026, 13:14Eirini Kontou: Launch of the e-Optimism Research Study to Support Life After TIA and Minor Stroke
-
Feb 13, 2026, 13:11Omar Adwan: Understanding ITP, TTP, and DIC
-
Feb 13, 2026, 13:01Abhishek Kumar: The Future of Uncontrolled Bleeding Therapies and the Evolving Hemostasis Pipeline
-
Feb 13, 2026, 12:49Simon Senanu: ‘Within Range’ Is Not the Same as ‘Safe’ in Laboratory Medicine
-
Feb 13, 2026, 12:35Heghine Khachatryan: Advances in Targeted Therapy Transforming TTP Management at ASH Highlights 2026
-
Feb 13, 2026, 12:03Prabineshwor Prasad Lekhak: Saving a Girl with Hemophilia When Every Drop Counts
-
Feb 13, 2026, 11:37Finn Guo: Access and Affordability Challenges for Von Willebrand Disease in China

