
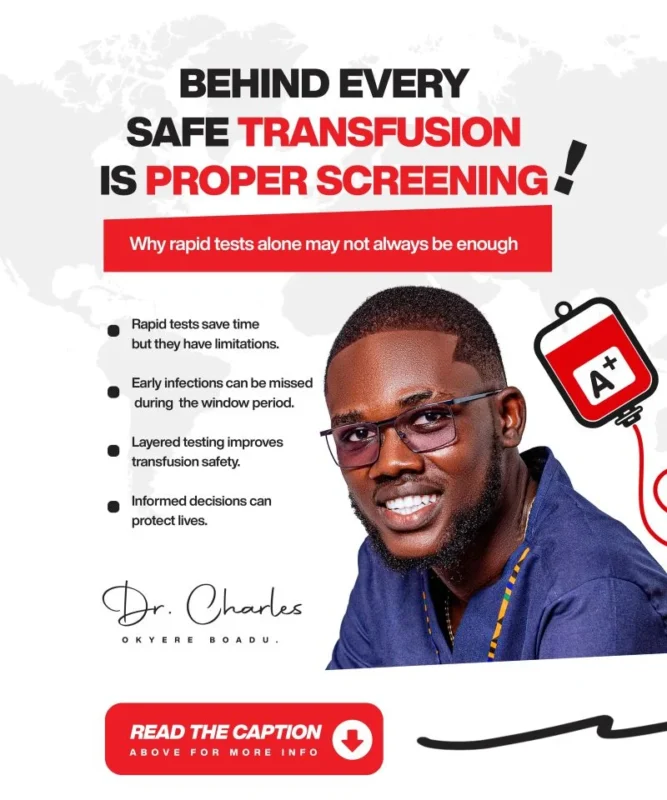
Charles Okyere Boadu: Safe Blood Saves Lives, Safer Blood Protects Futures
Charles Okyere Boadu, Medical Laboratory Science Student at the University for Development Studies, shared on LinkedIn:
”As a medical laboratory professional, I have come to appreciate how critical blood donor screening is to transfusion safety.
The primary responsibility of transfusion services is to ensure that blood released for transfusion is as safe as possible, since transfusion-transmissible infections remain a major public health concern.
In many health facilities, rapid diagnostic tests (RDTs) are routinely used to screen donated blood for transfusion-transmissible infections such as HIV, hepatitis B, hepatitis C, and syphilis. These tests are commonly employed in emergency situations and resource-constrained centers because they are easy to use and provide results quickly.
When RDT results are non-reactive and all other donor screening criteria are met, the blood is often considered safe and released for transfusion.
However, it is important to note that RDTs have limitations.
Although high-quality, validated RDTs can demonstrate excellent sensitivity, they may still fail to detect infection in certain situations.
When the level of analyte such as viral antigen or antibody is very low, particularly during early infection or the window period, the test may not detect it, resulting in a non-reactive result despite the presence of infection.
False-negative results may occur due to early testing, low viral load, viral variants, or other biological factors(Choudhary et al., 2025).
This is why I believe public awareness is crucial.
It could be me, you, or one of our relatives receiving blood someday. Whenever possible, especially before transfusion, it is reasonable to ask whether additional or confirmatory testing such as ELISA has been performed alongside RDT screening.
ELISA is widely regarded as the gold standard for blood donor screening because it allows objective interpretation, quality control monitoring, and reliable detection of transfusion transmissible infections (Choudhary et al., 2025).
I understand that ELISA testing requires more time, and many patients who need blood are in critical condition where delays can be life-threatening.
Nevertheless, ensuring the highest possible level of blood safety remains essential, as a patient may receive blood, recover, and later develop an infection without ever knowing the source.
This is not to discredit RDTs. Rather, this is a call to encourage layered testing, appropriate use of confirmatory methods, and informed decision-making in transfusion practice, as integrating multiple testing strategies has been shown to improve overall blood safety.
Safe blood saves lives. Safer blood protects futures.”
Stay updated with Hemostasis Today.
-
Feb 10, 2026, 14:18Pierpaolo Di Micco: A Submerged Network Among Platelets and Infection
-
Feb 10, 2026, 14:12Luca Saba: Update of The Stroke Action Plan for Europe 2018–2030 Is Published in the European Stroke Journal
-
Feb 9, 2026, 17:43Radheshyam Meher: BLOOD-L-INK Vol. 1, Issue 2 is Now Live
-
Feb 9, 2026, 17:41Jim Hoffman: Affinity-Based Blood Purification as a Potential Alternative to Plasma Exchange
-
Feb 9, 2026, 17:17RishiRaj Sinha: Strengthening Donor Connections – A Forward Path for 2026, Insights From the Indian Subcontinent
-
Feb 9, 2026, 17:12Anna Randi: Latest VWD and Hemophilia A Research at EAHAD 2026
-
Feb 9, 2026, 17:08Gerard J Myers: Pulmonary Vascular Air Embolism in Mechanically Ventilated Newborn Infants
-
Feb 9, 2026, 16:50Save the Date for WSC 2026 in Seoul – World Stroke Organization
-
Feb 9, 2026, 16:44Rose Almashayekh: You Can’t Always See Health – Lessons from Marfan Syndrome

