Davide Stradella on Ischaemic Diseases of the Gastrointestinal Tract
Davide Stradella, Medical Director – Gastroenterology and Digestive Endoscopy at Mauriziano Hospital of Turin, shared on LinkedIn:
”Acute abdominal pain can be challenging.
Ischaemic disease could be a cause with wide range of severity where sometimes timing is fundamental.
Here’s a short clinical review (with graphic supported by AI)
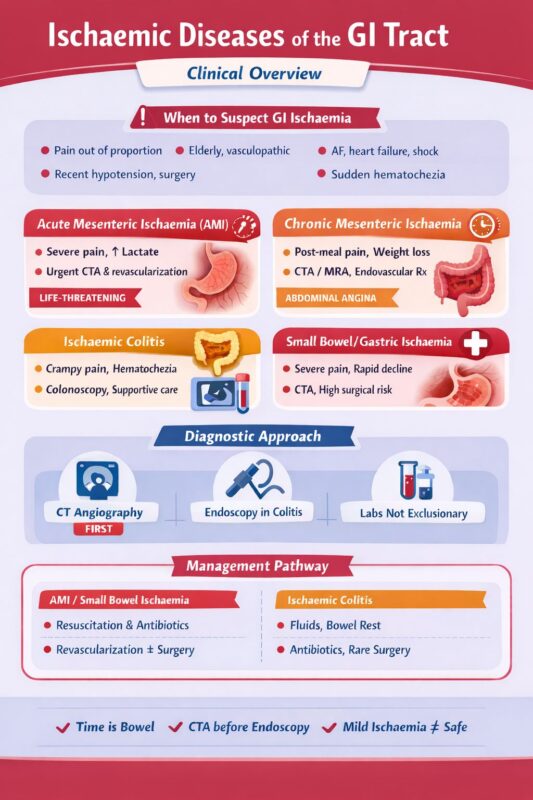
Ischaemic Diseases of the Gastrointestinal Tract
A practical clinical overview
Why it matters
GI ischaemia ranges from self-limited disease to life-threatening emergencies. Early recognition changes outcomes—especially in elderly, vasculopathic, or critically ill patients.
Main Entities (from top to bottom)
1. Acute Mesenteric Ischaemia (AMI)
The emergency
Mechanisms
• Arterial embolism (AF, cardiac sources)
• Arterial thrombosis (atherosclerosis)
• Non-occlusive mesenteric ischaemia (NOMI – shock, vasopressors)
• Mesenteric venous thrombosis
Clinical red flags
• Severe abdominal pain out of proportion to exam
• Metabolic acidosis, ↑ lactate
• Rapid progression to peritonitis
Diagnosis
• CT angiography (gold standard)
• Labs are supportive, not diagnostic
Management
• Immediate resuscitation
• Broad-spectrum antibiotics
• Revascularization (endovascular or surgical)
• Early surgery if bowel necrosis suspected
Delay equals bowel loss + high mortality
2. Chronic Mesenteric Ischaemia
“Abdominal angina”
Typical patient
• Elderly, smoker, diffuse atherosclerosis
Key features
• Post-prandial pain
• Fear of eating → weight loss
• Diarrhea or bloating
Diagnosis
• CTA or MRA
• Duplex US as screening
Treatment
• Revascularization (endovascular first-line)
• Risk factor control
3. Ischaemic Colitis
The most common GI ischaemia
Triggers
• Hypotension, dehydration
• Heart failure, dialysis
• Drugs (NSAIDs, vasoconstrictors)
• Post-operative states
Clinical presentation
• Crampy abdominal pain
• Acute hematochezia
• Left-sided predominance (watershed areas)
Endoscopic findings
• Segmental erythema
• Edema, petechiae
• Cyanosis or ulcerations in severe cases
Management
• Supportive (IV fluids, bowel rest)
• Antibiotics if moderate–severe
• Surgery only if necrosis/perforation
Most cases are reversible if recognized early
4. Small Bowel Ischaemia
Often underdiagnosed
Causes
• Mesenteric thrombosis
• NOMI
• Strangulation, volvulus
Clues
• Severe pain, minimal early findings
• Rapid deterioration
Diagnosis
• CTA
• Limited role for endoscopy
5. Gastric and Duodenal Ischaemia
Rare but severe
Associated with
• Shock
• Severe atherosclerosis
• Vasculitis
Endoscopy
• Pale or necrotic mucosa
• Ulcers with sharp demarcation
Clinical Take-Home Messages
• Pain out of proportion equals think mesenteric ischaemia
• Normal labs do NOT exclude ischaemia
• CTA is the diagnostic cornerstone
• Time is bowel (and life)
• Ischaemic colitis is often benign—but not always
Biblio
-ACG Guideline: Colon Ischemia, 2015
-ESVS Guidelines: Mesenteric Ischaemia, 2017
-ACR Appropriateness: Acute Abd Pain, 2022
-UpToDate: Mesenteric Ischemia
-Brandt LJ. NEJM Ischemic Colitis”
Stay updated with Hemostasis Today.
-
Jan 22, 2026, 15:36We Must Roll Up Our Sleeves And Help: José Antonio García Erce on Plasma Donation
-
Jan 22, 2026, 15:25Nita Radhakrishnan on Challenges In Congenital Afibrinogenemia
-
Jan 22, 2026, 15:10Jin Q Gives a Summary of 2025’s Most Impactful Cell and Gene Therapy Milestones
-
Jan 22, 2026, 14:57Nirav Dhanesha on CD14 Acting As A Functional Driver of DVT
-
Jan 22, 2026, 11:41Jamilla Goedegebuur and Colleagues on VTE Management in Case of PAD
-
Jan 22, 2026, 11:28Abdulrahman Katib on API-CAT Trial’s Evaluation of Apixaban Dosing
-
Jan 22, 2026, 11:19Bruno Odisio: Ablation Margins Are Software-Dependent
-
Jan 22, 2026, 10:38Pedro Perez: The VTE Market Is Clearly Entering Its Next Phase
-
Jan 22, 2026, 10:29Marvin Garcia Reyes Presents a Case of Aorto-Visceral and Aorto-Iliac Thrombosis
