Salvatore Massimo Petrina: High D-Dimer, Negative CT Scan – What’s Your Next Move?
Salvatore Massimo Petrina, Hospital Physician Cardiology ASP Ragusa, shared on LinkedIn:
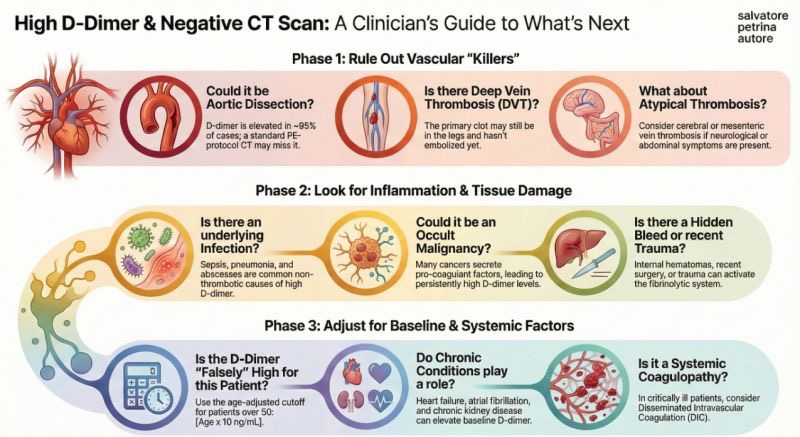
”Title: High D-Dimer, Negative CT Scan: What’s Your Next Move?
It’s a scenario every clinician knows well: a patient has a high D-dimer, you order a CT to rule out PE, and the scan comes back negative.
Do you discharge the patient and breathe a sigh of relief?
Not so fast.
A negative CT is a crucial data point, but it’s not always the end of the diagnostic journey.
A high D-dimer is a non-specific marker of coagulation activation, and we have a responsibility to investigate further.
This guide provides an excellent 3-phase framework for navigating this clinical puzzle:
Phase 1: Rule Out Other Vascular Risks
Before moving on, double-check for other life-threatening conditions that could have been missed or present concurrently.
Aortic Dissection: A critical can’t-miss diagnosis.
Deep Vein Thrombosis (DVT): Was a DVT ruled out, or was the focus solely on the PE?
Other VTE Events: Consider less common thrombotic events.
Phase 2: Search for Inflammation and Injury
The D-dimer is often elevated due to significant systemic stress.
It’s time to broaden the differential.
Infection/Sepsis: A very common cause of high D-dimer levels.
Occult Malignancy: Always consider this, especially in patients with no prior history.
Covert Bleeding or Trauma: Look for internal bleeding or injuries that aren’t immediately obvious.
Phase 3: Adjust for Baseline and Systemic Factors
Sometimes, the high D-dimer reflects the patient’s chronic state rather than an acute event.
Chronic Inflammation: Conditions like rheumatoid arthritis or IBD.
Systemic Coagulopathies: Underlying clotting disorders.
Patient-Specific Factors: Advanced age or post-surgical state can keep levels elevated.
The key takeaway: A high D-dimer is a signal to keep looking.
A systematic approach ensures we don’t stop our search prematurely and provide the best care for our patients.
How do you approach this situation?
Share your clinical pearls and go-to differentials below!”
Stay updated with Hemostasis Today.
-
Feb 19, 2026, 16:01Honoring Black Pioneers in Hematology During Black History Month – ASH
-
Feb 19, 2026, 15:16Irina Pahlevanyan: Global Leaders on Courage, Trust, and the True Purpose of Fundraising
-
Feb 19, 2026, 15:12Stéphanie Forté: Transition Readiness in Youth With Sickle Cell Disease
-
Feb 19, 2026, 15:08Tagreed Alkaltham: Strengthening Blood Inventory Governance Through RFID Technology
-
Feb 19, 2026, 14:59Başak Taburoğlu Yılmaz: Improving Diagnosis and Care for Women With Bleeding Disorders
-
Feb 19, 2026, 14:59Munira Borhany: Moving Beyond Stereotypes in the Diagnosis of Bleeding Disorders
-
Feb 19, 2026, 14:56Flora Peyvandi: Personalized VWF Dosing Revolutionizes Surgery in VWD
-
Feb 19, 2026, 14:54Michela Mazzon: The Molecular Trigger Behind the COVID19 Vaccines-Associated ITT
-
Feb 19, 2026, 14:42Luca Palombi: Real-Time Assessment of Venous Hemodynamics During Movement With DUS

