
Non-Invasive Management of Radial Artery Pseudoaneurysm
Aren Mnatzakanian, Researcher at Breast Imaging Research Consortium, shared a post on LinkedIn:
“In our latest “Lessons in IR” paper published in JVIR, we described the non-invasive management of a rare iatrogenic complication of transradial access, radial artery pseudoaneurysm (RA-PSA). We provide the following insights into how to anticipate, prevent and manage this complication.
Case
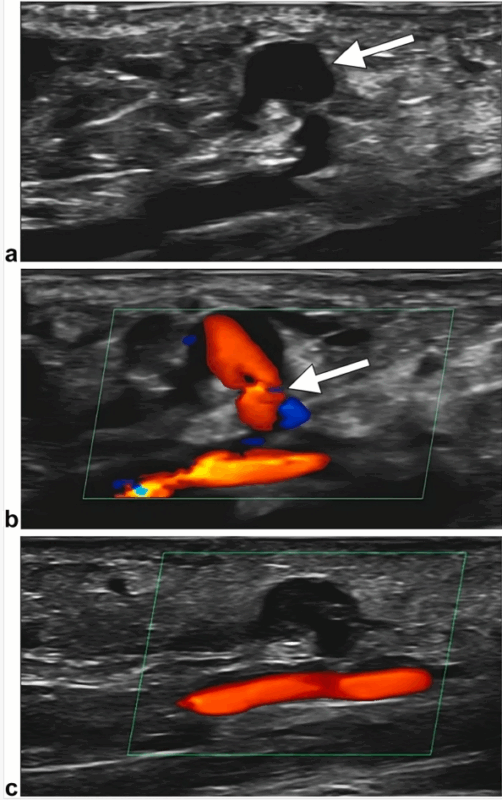
The day after successful rental artery stenting via left transradial access, our patient developed a pulsatile mass at the puncture site. Doppler US showed a 9 × 7–mm saccular outpouching of the superficial radial artery wall (arrow, Fig 1a) with turbulent flow through a narrow 2-mm neck (arrow, Fig 1b), consistent with pseudoaneurysm. To attempt non-invasive management, the skin overlying the lesion was marked under US guidance. A TR Band was applied directly over the pseudoaneurysm and inflated with 12 mL of air (nonocclusively) for 48 hours, allowing sufficient time for immobilization and spontaneous thrombosis. Follow-up Doppler US confirmed complete thrombosis with patent parent artery (Fig 1c). Recovery was uneventful.
Preparation
- Patient risk factors for radial artery pseudoaneurysm (RA-PSA) include older age, vessel calcification, anticoagulant/antiplatelet use, and coagulopathy.
- Procedural risk factors include repeated punctures, catheter infection, larger sheath size, longer procedure, and incomplete hemostasis.
- Identify high-risk patients as they may require prolonged compression and closer postprocedural monitoring.
Avoidance
- Society of Interventional Radiology (SIR) Quality Improvement Standards report RA-PSA rate of 0.5% (0–0.72%) with quality index threshold 1.2%; higher rates require audit.
- Perform the Barbeau or modified Allen test before the procedure to assess collateral hand circulation.
- Ensure artery-sheath compatibility with preprocedural US (anteroposterior diameter, inner-to-inner wall).
- Monitor postprocedural radial pulse, plethysmography, pain, weakness, discoloration, reduced temperature, and sensory deficits in the hand/fingers.
Management
- Treatment of pseudoaneurysms is guided by size, location, aneurysm neck and symptoms, distal circulation, and presence of thrombus.
- Nonsurgical options include manual or US-guided probe compression, nonocclusive hemostatic cuffs (eg, TR Bands), and image-guided thrombin injection.
- Titrate volume of TR Band after achieving occlusive hemostasis by withdrawing 1 mL/s of air until pulsatile bleeding is observed at the access site, followed by injection of 1–2 mL until bleeding stops.
- Surgical repair is indicated for large or rapidly expanding RA-PSA, unsuccessful conservative management, infection, distal hand ischemia, and compressive neuropathy of the radial or median nerves.”
Stay updated with Hemostasis Today.
-
Feb 25, 2026, 13:36Zoltan Nagy: Antibody Response Can Shift from Recognizing the Adenoviral Protein to Targeting PF4 in Rare VITT Cases
-
Feb 25, 2026, 13:08Sam K. Saha: Same Clot Against Fast and Slow Systems
-
Feb 25, 2026, 13:04Haykaz Muradyan: The Use of REBOA in Obstetric Haemorrhage
-
Feb 25, 2026, 12:53Jan Hartmann: NexSys Plasma Collection System Receives FDA Clearance
-
Feb 25, 2026, 12:45Zain Khalpey: Secondary Stroke Prevention as The Most Important Opportunity to Reduce Disability
-
Feb 25, 2026, 12:40Jeff June: Stroke Care Is Clinically Mature, Stroke Biology Is Still Evolving
-
Feb 25, 2026, 12:36Wolfgang Miesbach: Repurposing Metformin – From Sugar Control to Thrombus Control
-
Feb 25, 2026, 12:30Bethany Brown: There Is A Need for A Validated Replacement for The Discontinued 2,3-DPG Assay
-
Feb 25, 2026, 12:20Register for A Webinar on von Willebrand Disease in Ageing – EHC

