Benedikt Lorenz on Liver Failure and Coagulation – Myths, Traps, and Bad Habits
Benedikt Lorenz, Senior Physician, Interdisciplinary Surgical Intensive Care Medicine at Schleswig-Holstein University Hospital, shared on LinkedIn:
”Liver failure and coagulation – myths, traps, and bad habits.
Liver failure and hepatic insufficiency cause profound changes in standard lab tests — and anyone treating these patients must know the pitfalls.
A colleague asks whether to give PCC before inserting a Shaldon catheter for ADVOS therapy in a patient with right heart failure and liver failure.
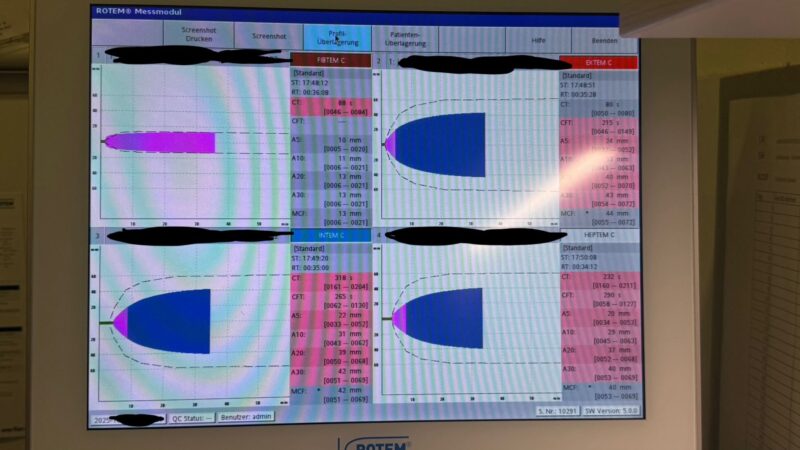
“We never give PCC blindly – except
A) if a patient is on warfarin and bleeding, or
B) if the ROTEM shows a prolonged CT in the EXTEM after (!) correction of hypofibrinogenemia and/or thrombocytopenia!”
This patient with a Quick of 26% and INR 2.46 must not receive PCC — the clotting time is perfectly normal.
If this patient bleeds, he needs fibrinogen concentrate (never plasma or whole blood – hypervolemia only makes things worse! [portal hypertension]).
Even platelet transfusion must be considered carefully: in thrombocytopenic liver failure, VWF levels rise and ADAMTS13 activity falls, creating a prothrombotic state despite low platelet counts.
It becomes tricky, as here, after cardiac surgery, when platelet function is already impaired.
Treat first what kills first!
Coagulation therapy must be individualized – there is no one-size-fits-all recipe.
Giving PCC in this context means risking thromboembolic events, jeopardizing vascular anastomoses after liver transplantation or generally in surgery, and clogging oxygenators in ECMO or other extracorporal therapies like ADVOS oder hemodialysis circuits.
Everyone who has ever transplanted a liver knows: there is no correlation between Quick/INR and bleeding – but a very real one between PCC and thrombosis while it is super effective in patients who really need it.
And one day, even our friends in trauma surgery across the Atlantic will understand:
A low Quick is not a coagulopathy to be fixed with PCC (that’s why it doesn’t work in your studies)– it’s the footprint of hypofibrinogenemia or thrombocytopenia.
The only reliable guide in these patients? Thromboelastography.
The only reliable therapy in these patients? Pure factor concentrate.”
Stay updated with Hemostasis Today.
-
Dec 15, 2025, 12:46Deborah Ebert Long on Hemophilia Care: Progress, Possibility, and the Power of Listening
-
Dec 15, 2025, 12:34Nathan Connell on Conversion from Eptacog Alfa to Beta
-
Dec 15, 2025, 12:17Danny Hsu on Interdisciplinary Toolkit for Gynecologic Bleeding on Anticoagulation
-
Dec 15, 2025, 12:08Ted Roh: A Historic Milestone for Indonesia’s Health Innovation
-
Dec 15, 2025, 11:28Wolfgang Miesbach Shares Insights from Davide Matino’s Presentation on Marstacimab at ASH25
-
Dec 15, 2025, 11:12Tushar Pandey Awarded for His Enourmous Contribution to Hematology
-
Dec 15, 2025, 11:07DISTRO: Vidya Rajbhoj on AI and Digital Technology to Improve Stroke Rehabilitation
-
Dec 15, 2025, 11:00Ischemic Stroke, AF and Atherosclerotis: Amira Khater on Sufficiency of Anticoagulant Monotherapy
-
Dec 14, 2025, 16:06Dr Abdul Mannan: What’s Your Approach to Diagnosing Iron Deficiency in Tricky Cases?