
Abdul Mannan: When Blood Clots Show Up in Unexpected Places
Abdul Mannan, Consultant Haematologist at Betsi Cadwaladr University Health Board, shared a post on LinkedIn:
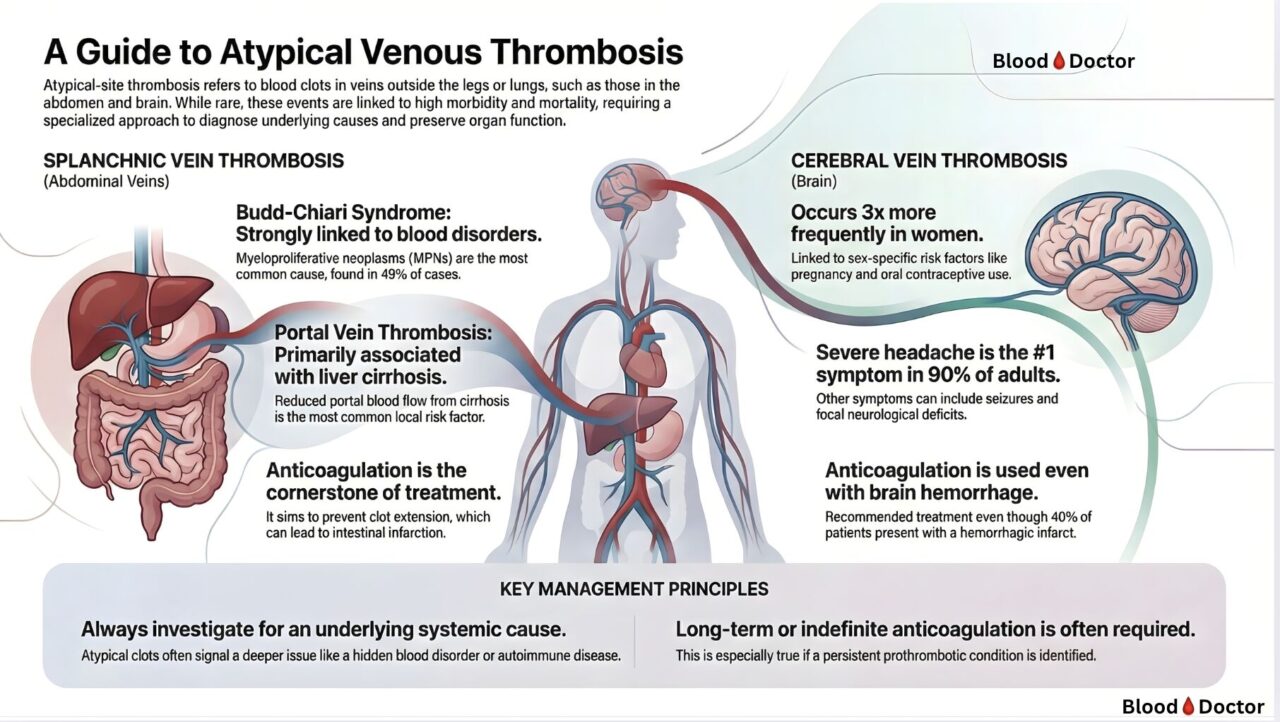
“When Blood Clots Show Up in Unexpected Places
Most doctors think DVT and PE when they hear ‘blood clot.’
But as a Thrombosis Lead, I spend a lot of time managing clots that don’t follow the textbook. The ones that form in the brain. In the liver veins. In the portal system.
These are the cases that keep haematologists busy — and they demand a completely different mindset.
Let’s talk about two locations that matter:
Splanchnic Vein Thrombosis (Abdomen)
When I see Budd-Chiari syndrome, my first question isn’t “why did this clot form?”
It’s “which myeloproliferative neoplasm am I going to find?”
Because MPNs account for nearly half of all cases. That’s 49%. And here’s the thing — sometimes the clot appears before any other sign of the blood cancer. The thrombosis IS the presentation.
Portal vein thrombosis tells a different story. Liver cirrhosis dominates here. Sluggish flow. Damaged vessels. The perfect storm for clot formation.
In both scenarios, anticoagulation remains the treatment backbone — even when it feels counterintuitive. Without it, clot extension leads to intestinal infarction. And that’s a disaster.
Cerebral Vein Thrombosis (Brain)
Three times more common in women. Pregnancy. Oral contraceptives. The hormonal connection is undeniable.
90% present with severe headache. Not a mild one — the kind that brings patients to A&E thinking the worst.
Now here’s what surprises many colleagues:
We anticoagulate even when there’s hemorrhage on imaging.
Yes, you read that right. About 40% of CVT patients have hemorrhagic transformation at diagnosis. We still anticoagulate. The evidence supports it. The clot needs treatment, and the bleeding is usually a consequence of venous congestion, not arterial rupture.
Two principles I live by:
1. Always hunt for the underlying cause. Atypical clots are often the tip of the iceberg. MPNs. Paroxysmal nocturnal haemoglobinuria. Antiphospholipid syndrome. Behçet’s disease. Don’t stop until you’ve looked.
2. Think long-term. These aren’t your standard three-month anticoagulation cases. When we find a persistent prothrombotic condition, indefinite treatment becomes the conversation.
Atypical site thrombosis is rare. But when it happens, getting it right changes lives.
Have you encountered challenging atypical thrombosis cases? What was the underlying diagnosis?”
Find more posts featuring Abdul Mannan on Hemostasis Today.
-
Jan 27, 2026, 14:06Dmitrii V Kalinin Shares A PhD Opportunity: Hardiman Scholarship
-
Jan 27, 2026, 13:48Filippo Cademartiri: 3 Biomarkers Are Better Than 1: Refining ASCVD Risk in MESA
-
Jan 27, 2026, 12:27Martin Haluzík on Residual Cardiovascular Risk in Coronary Artery Disease
-
Jan 27, 2026, 12:18Stuart Phillips: Strong Bodies Are Good, Informed Bodies Are Better!
-
Jan 27, 2026, 12:07Daniel Torrent: This Should Be An Ice Cold Take… But Veins Aren’t Arteries
-
Jan 27, 2026, 09:17Paolo Zamboni on CCSVI Associated to Multiple Sclerosis
-
Jan 27, 2026, 09:02Rowan Paul: Platelet Dose Determines Success in PRP Therapy
-
Jan 27, 2026, 08:48Uriel Suárez: Hemi‐Orolingual Angioedema in a Patient With VEXAS Syndrome
-
Jan 27, 2026, 08:23Rossella Crescitelli on Platelets’ and PEVs’ Association with Lung Cancer Metastases
