Hematology vs Oncology: Why They Often Go Together
At first glance, hematology and oncology appear to occupy separate intellectual territories: one rooted in the physiology of blood and marrow, the other organized around solid tumors and organ-based disease. This distinction gives rise to a perceived “hematology vs oncology” dichotomy. However, the increasing understanding of cancer pathophysiology has progressively blurred the boundaries, particularly in the study and management of blood malignancies, which share mechanisms with solid tumors yet require hematologic expertise. This has led to the combined discipline of hematology-oncology, which plays a central role in modern cancer care.
This review smoothly sets up the “vs” while exploring the “together”, and briefly dives into the traditional scope, history, rationale, and overarching challenges.
Why Understanding the Difference Matters
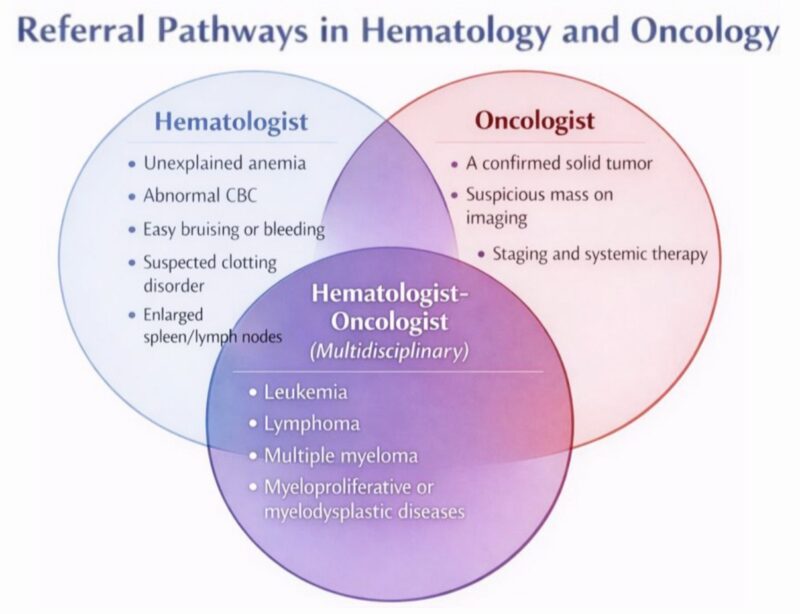
Understanding the differences helps patients navigate their care teams, know why they are referred to one specialist versus another, and understand the nature of their condition-blood disorder, cancer or both.
Hematology and oncology can be combined or pursued separately. Knowing the differences helps medical students choose between benign hematology, malignant hematology, solid-tumor oncology, or combined heme-onc practice, each with different workloads, research opportunities, and clinical focus.
Hematology encompasses a wide spectrum, spanning molecular mechanisms of blood cell formation to diseases of the blood, bone marrow, and lymphatic system. Hematologists diagnose and guide therapy for disorders ranging from anemias and hemostatic abnormalities to malignant conditions such as leukemias.
Oncology focuses on the study, diagnosis and management of malignant diseases. Oncologists examine how and why cells become malignant. Guided by tumor histology, molecular markers, and staging, they utilize surgical, radiation, and systemic therapies to halt or reverse the course of disease.
What Are the Core and Emerging Areas Within Hematology
Diagnostic hematology remains a core component of the specialty.
It encompasses:
- Morphologic interpretation of peripheral blood smears and bone marrow specimens. Hematologists continue to serve as the bridge between classical microscopy and modern molecular data, contextualizing each within the patient’s clinical picture.
- Flow cytometry, which enables immunophenotypic classification of leukemias and lymphomas, minimal residual disease (MRD) assessment, and quantification of immune subsets. Hematologists participate in gating strategies, and interpretation of high-parameter panels.
- Specialized Coagulation and hemostasis diagnostics. Hematologists interpret these in tandem with genetic panels for thrombophilia or bleeding disorders, ensuring clinically meaningful evaluation.
- Molecular hematopathology incorporation of technologies like FISH, PCR immunohistochemistry, cytogenetics, and next-generation sequencing (NGS) panels. Hematologists are now expected to understand variant classification, clonal architecture, allele burden trends, and the clinical relevance of actionable mutations, which redefines the diagnostic responsibilities.
Clinical hematology covers the full spectrum of management, and monitoring of blood-related diseases.
Benign hematology is a subspecialty domain, where hematologists manage red cell disorders (hemolytic and dyserythropoietic anemias, hemoglobinopathies), platelet and hemostatic abnormalities (thrombocytopenia, inherited/acquired platelet function defects), coagulation disorders (hemophilias, VWD, thrombophilia, APS), bone marrow failure syndromes (aplastic anemia, PNH), and non-neoplastic white blood cell disorders. The examples listed here illustrate merely a fraction of the extensive array.
Transfusion medicine and cellular therapy:
Most hematologists maintain active roles in transfusion support, blood product stewardship, and management of transfusion complications. They also possess specialized expertise in immunohematology and blood compatibility.
In addition to traditional stem cell transplantation, the rise of CAR-T cells, gene-edited stem cells, and ex vivo-expanded cellular products has further expanded the hematologist’s responsibilities. They now oversee patient selection, toxicity management (CRS, ICANS) and long-term monitoring.
Within malignant hematology, clinicians diagnose and manage leukemias, lymphomas, myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPN), multiple myeloma, and other neoplasms. Cancer biology concepts such as clonal evolution, stem cell dysfunction, somatic mutations, epigenetic alterations were first described in hematologic malignancies. Because blood is uniquely accessible for sampling, hematology remains a prototype for translational precision medicine.
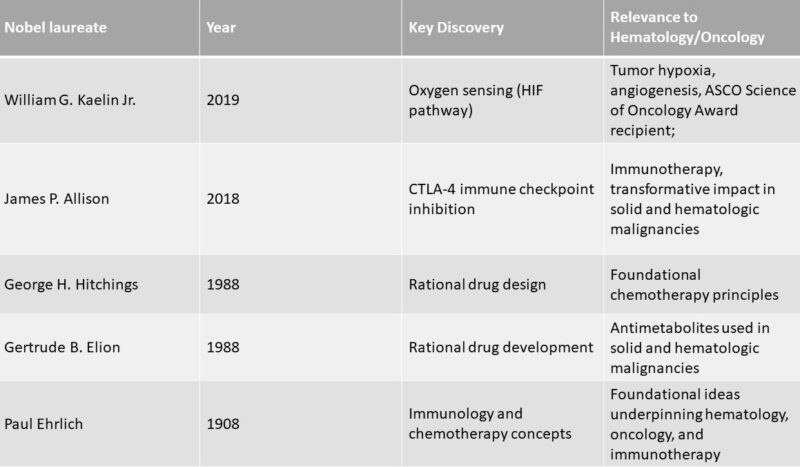
“Hematology vs Oncology”- Evolution
Post-World War II, hematology evolved from classical blood disorders toward cancer-focused investigations. As some hematologists refocused their work toward cancer, a number of internists became interested in the application of chemical therapies to solid tumors. However, they encountered antagonism, reflecting both professional territoriality and skepticism toward emerging therapeutic modalities. To circumvent these barriers, internists aligned with related fields or joined specialized cancer hospitals such as Memorial Sloan-Kettering or Roswell Park. They also formed a national society (ASCO) and developed standard training requirements-common expressions of the rise of specialization in the 20th century.
When medical oncologists claimed wide-ranging expertise over the treatment of all patients suffering from malignant disease, the leukemias became contested ground. At the annual meeting of the American Society of Hematology (ASH), and in a subsequent letter to the ABIM (American Board of Internal Medicine), hematologists declared- “The separation of the two boards is itself a denial of the capabilities and dedication of a large number of practicing hematologists to the care of patients with neoplastic disease.”
This led to a structured negotiation: the development of dual certification and joint training programs, a compromise that preserved hematologists’ involvement while establishing medical oncology as an independent subspecialty.
By the late 1970s, medical oncology had secured institutional legitimacy. Hematology-oncology relations evolved from conflict to structured cooperation, though tensions over training and certification persisted. The ABIM revised its training requirements. Candidates who had focused primarily on hematology required an additional year in oncology, those with an oncology background needed 2 years in hematology, and those from a combined program completed 3 years of training.
The Growing Overlap
Molecular oncology and NGS-based comprehensive sequencing have reshaped classification systems, particularly in MDS and acute leukemias, and now guide therapy across solid and hematologic cancers. Tumor mutational profiling, minimal residual disease tracking, and liquid biopsy technologies are expanding across both specialties.
Contemporary master protocol frameworks such as basket and umbrella trials, often combine hematologic and solid tumors, particularly when targeting common molecular alterations. Basket trials, for example, enroll patients with a shared actionable genomic aberration (such as BRAF V600E, NTRK fusions, IDH1/2 mutations), across diverse cancer types, thereby evaluating a single targeted therapy in a histology-agnostic manner. In a systematic review, 180 basket trials were identified, with 55 % reporting results and a median objective response rate of 14 %.
Umbrella trials complement this approach by stratifying patients with a single disease (for instance acute leukemia or non-small cell lung cancer) into molecularly defined sub-cohorts that receive different targeted agents. Of 73 umbrella trials evaluated, 38 % had published outcomes with a median response rate of 17.8 %. (Olivier et al, 2023)
CAR-T, bispecific T-cell engagers (BiTEs), and NK-cell therapies were pioneered in blood cancers and now illustrate how treatment approaches cross specialty boundaries (although their global availability remains uneven, contributing to substantial disparities in care). At the same time, conventional oncology modalities (chemotherapy, radiation) and hematology treatments (stem-cell transplant, supportive transfusion care, anticoagulation) are often used together in combined care pathways.
Workforce shortages amid an increasing number of new cases
Latest global estimates from IARC GLOBOCAN 2022 highlight the growing burden of cancer (20 million new cancer cases and 9.7 million deaths) and the disproportionate impact on underserved populations. These increases are mostly due to population aging and growth, not changes in individual risk alone. Hematologic malignancies accounted for 6.6% of total cancer cases (non-Hodgkin lymphoma exhibits the highest incidence) and 7.2% of total cancer-related deaths (leukemia has the highest mortality rate). WHO survey (2022) on UHC and cancer shows that only 39% of participating countries covered the basics of cancer management as part of their financed core health services for all citizens.
A new (2025) report from the American Society of Clinical Oncology finds that the overall density of medical and hematology oncologists relative to the aging population is decreasing. In 2014, there were an estimated 15.9 oncologists per 100,000 people aged 55 and older, that number dropped to 14.9 in 2024. Data identify significant “cancer care deserts,” particularly in rural communities. By 2037, non-metropolitan areas are projected to meet only 29% of their demand for medical and hematology oncologists, contrasting with metropolitan areas which are projected to meet 102% of their demand.
Residency Experience and Academic Outlook
Interest in combined hematology-oncology fellowships continues to grow compared with hematology-only or medical-oncology-only programs. NRMP (the National Resident Matching Program) data tables show that the number of hematology-oncology programs has increased from ~149 in 2019 to around 198 by the 2024 appointment year, with 773 certified positions (fill rate was 99%). According to Mosquera et al.’s 2024 study, factors influencing career choice included clinical interest in the field (98%), previous research experience in HO, career mentorship, lifestyle considerations, and perceived job market.
However, a central challenge of the model lies in the breadth and complexity of knowledge required to practice competently across both domains. Benign hematology-often less procedurally oriented and less commercially supported-risks marginalization, raising concerns about workforce preparedness to manage non-malignant blood disorders.
Recruitment into academic medicine is a problem faced by all medical specialties. A 2025 national survey of U.S. hematology/oncology fellowship leaders found that about one-third of trainees pursue community-based careers despite training in academic centers. While most leaders agree that fellowship programs should prepare trainees for community practice, non-clinical career skills remain insufficiently covered.(Agrawal et al., 2025)
There is an increasing emphasis each year on the advancement of scientific research in Armenia. This emphasis is reflected in the heightened engagement of professionals in conducting and participating in clinical trials, attending international scientific events, and fostering the promising careers of young specialists. Armenian hematologists-oncologists are also striving to make contributions to global medical and scientific endeavors. In this context, it is worth mentioning the commencement of the blastic plasmacytoid dendritic cell neoplasm (BPDCN) international registry in 2022, initiated by the Immune Oncology Research Institute, which is the only similar initiative globally. (Movsisyan et al., 2024)
Many physician-scientists ultimately choose hematology/oncology because of the rapid pace of scientific advances and the opportunities for biomedical research. In addition to traditional bench (“wet lab”) research, many focus on computational biology and health services (“dry lab”) work. Reviews on ASH educational resources detail how research priorities (bioinformatics, RWD, AI) reshape clinical expectations.
The key points are
- Many “cancers” originate in blood, bone marrow, lymphatic system so “cancer care” and “blood-system medicine” naturally overlap.
- Shared diagnostic and therapeutic strategies, along with novel approaches, make this integration even more logical.
- Combined hematology-oncology services improve efficiency, reduce fragmentation of care, and facilitate multidisciplinary management.
Read the full article for a comprehensive overview of hematologic oncology in Armenia, published in the OncoDaily Medical Journal (ODMJ).
News posts featuring ASH 2025 on Hemostasis Today.
Written by Susanna Mikayelyan, MD.
FAQ
Is hematology the same as oncology?
No. Hematology focuses on blood disorders, while oncology focuses on cancer. They overlap in blood cancers.
Do all cancers fall under oncology?
Yes, but blood cancers fall under both oncology and hematology.
Are hematologists also oncologists?
Often yes-many physicians train in both fields.
Is hematology part of oncology?
They are separate specialties but overlap substantially, many physicians practice as hemato-oncologists because blood cancers require combined expertise.
Who is a hemato-oncologist?
A physician trained to diagnose and treat both blood disorders and cancers, often handling complex cases that sit at the intersection of both fields.
-
Feb 17, 2026, 09:04Mahesan Subramaniam: A Heart Attack Is a Long Story That Ends Fast
-
Feb 16, 2026, 15:44Lakmali Silva: Silva Lab Showcases Research at the Gordon Research Conference on Plasminogen and Extracellular Proteolysis
-
Feb 16, 2026, 15:36Heghine Khachatryan: Strengthening Maternal Resilience Against Postpartum Hemorrhage
-
Feb 16, 2026, 15:34Sevak Mirabyan: Advancing Cancer Care Through Knowledge, Collaboration, and Early Diagnosis in Armenia
-
Feb 16, 2026, 15:29Chokri Ben Lamine: Key Clinical Insights of Drug Induced Thrombocytopenia
-
Feb 16, 2026, 15:28Ney Carter Borges: Coronary Intravascular Lithotripsy – Clinical Performance and Safety
-
Feb 16, 2026, 15:24Flora Peyvandi: Highlighting Overdose, Homicide, and Suicide as Causes of Maternal Death in the US
-
Feb 16, 2026, 14:53Wafaa Abougabal: Differential Diagnosis of Acute Neurologic Deficits and Stroke in PICU
-
Feb 16, 2026, 14:49Nayab Ahmed: Synthesis of ATP and Its Significance in Storage of Blood

