
Ashok Yadav Explains Fetal Thrombotic Vasculopathy: FTV
Ashok Yadav, Biology Educator of Biology Faculty at Apex Academy, shared on LinkedIn:
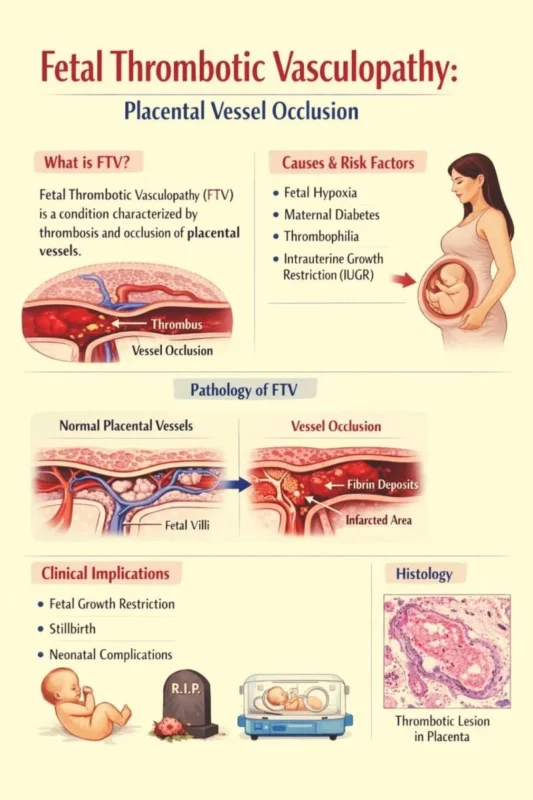
”Fetal thrombotic vasculopathy (FTV) – what every obstetric, neonatal and pathology team needs to know
1. What it is
A placental fetal-side clotting disorder that produces:
– Occlusive or mural thrombi in chorionic plate / stem villous vessels
– Downstream ischemia → villous stromal-vascular karyorrhexis → avascular villi
2. How we diagnose it (Society-of-Paediatric-Pathology criteria)
Need at least 2 foci, each averaging ≥ 15 contiguous terminal villi:
– Avascular villi – fibrotic ghost villi with zero fetal capillaries
– Villous stromal karyorrhexis – fragmented RBCs and nuclear debris in villous stroma (intermediate stage)
Optional corroborative clues:
– Thrombus in a large fetal vessel (often laminated, septated, mineralised)
– Focal stem-vessel obliteration (fibro-connective tissue replacing vessel lumen)
3. Gross placental hints (subtle – easily missed)
Early: wedge-shaped pale, soft areas
Late: grey-white firm patches that can mimic maternal infarcts
Cord abnormalities or true knots are frequent co-findings
4. Why it matters – neonatal and obstetric correlates
Severe FTV correlates with:
– IUGR / small-for-gestational-age
– Intracranial haemorrhage, neonatal coagulopathy
– Hypoxic-ischaemic encephalopathy / cerebral palsy
– Pre-term delivery for fetal indications, oligohydramnios, stillbirth
– Later evidence of systemic thrombosis / pro-thrombotic state
5. Differential diagnoses – don’t be fooled
– Intra-uterine fetal demise – diffuse, same-age vascular changes; no clustered avascular villi
– Chronic villitis – lympho-histiocytic infiltrate, inflammation in vessel wall
– Mesenchymal dysplasia – hugely dilated vessels plus hydropic villi; no uniform thrombi
– Maternal villous infarct – collapsed inter-villous space, trophoblast necrosis, villi stuck together
6. Ultrasound / in-utero imaging
FTV itself is not reliably seen on routine US; clues are indirect:
– Placental heterogeneity, echogenic intravascular dots (suggest thrombus)
– IUGR, abnormal Doppler (raised PI, absent/reverse end-diastolic flow)
– Hydrops, oligohydramnios, or thrombus in fetal IVC / renal veins on targeted scan
7. Work-up after diagnosis
– Examine infant for thrombosis (renal, CNS, IVC)
– Consider pro-thrombotic testing for baby and mother (factor V Leiden, prothrombin G20210A, APLA, etc.)
– Neurological follow-up – FTV is a recognised precursor of perinatal stroke and cerebral palsy
8. Key take-home
Think of FTV whenever the placenta shows clustered avascular villi or villous karyorrhexis; recognise its link to fetal hypoxia, IUGR and long-term neuro-disability; rule out mimics by pattern and distribution; use the diagnosis to trigger both neonatal surveillance and family thrombophilia screening.”
Stay updated with Hemostasis Today.
-
Jan 30, 2026, 11:38Aaron Rodriguez Calienes on Intracranial Stenting: Rescue vs First-Line Outcomes
-
Jan 30, 2026, 11:25Ahmed Nasreldein on Sex Disparities in Thrombolysis Delay Among Egyptian Stroke Patients
-
Jan 30, 2026, 11:17Yanki Yarman: My PhD Project Has Been Published in Blood!
-
Jan 30, 2026, 11:08Alexandros Apostolou on Complications Associated with IDU and Thrombophilia
-
Jan 30, 2026, 10:57Peisong Ma on GRK5 Polymorphism Affecting Platelets
-
Jan 30, 2026, 10:34Saif ur Rahman Compares K2 and K3 EDTA: Key Differences Explained
-
Jan 30, 2026, 10:22Manpreet Gill on Heparin Resistance: When 14 Years of Experience Finally Gets a Plot Twist
-
Jan 30, 2026, 10:14Mohamed Elsaid on The Role of Hyperlipidemia in Thrombogenesis
-
Jan 30, 2026, 09:57From Risk Visualization to Plaque Change: Babak Alex Vakili on CAC and CCTA Insights
