
Ahmad Ibrahim Ahmad Zainuddin: Aspirin in Primary Prevention Is Now a Carefully Selected Exception
Ahmad Ibrahim Ahmad Zainuddin, Medical Advisor and Occupational Health Doctor at eBen Assist Sdn Bhd, shared on LinkedIn:
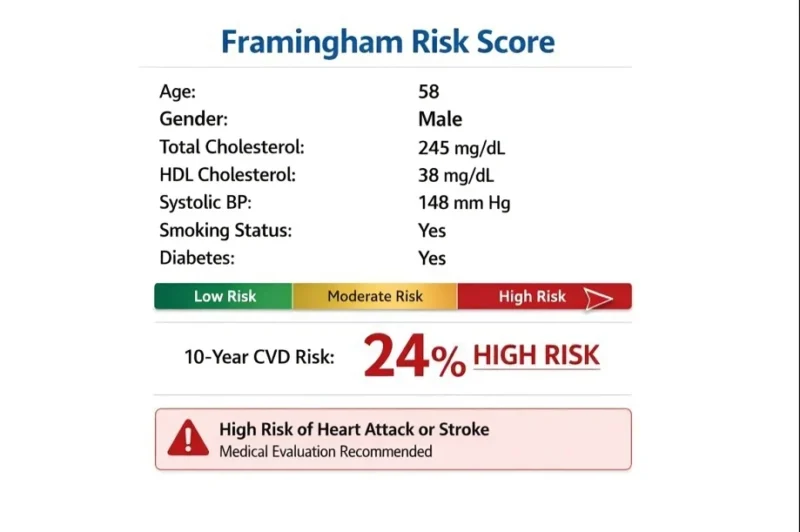
“A client asked me recently, ‘If someone is high risk for cardiovascular disease, should we start aspirin for primary prevention?’
For years, aspirin symbolized proactive medicine. One small tablet to prevent the first myocardial infarction or stroke. It felt logical, accessible, and safe.
But modern evidence tells a more nuanced story.
The ASCEND trial showed that in patients with diabetes, aspirin reduced serious vascular events (8.5% vs 9.6%) but increased major bleeding (4.1% vs 3.2%) (ASCEND Study Collaborative Group, NEJM, 2018).
The ASPREE trial found no cardiovascular mortality benefit in healthy older adults, yet bleeding risk rose significantly (McNeil et al., NEJM, 2018).
A meta-analysis of over 160,000 patients captured the dilemma clearly. The absolute reduction in cardiovascular events was about 0.4%, while major bleeding increased by roughly 0.5% (Zheng et al., JAMA, 2019).
Nearly symmetrical benefit and harm.
Why did aspirin lose its preventive dominance?
Because cardiovascular prevention improved. Blood pressure is treated earlier, statins are widely used, diabetes care is more cardioprotective, and smoking rates have declined. When baseline risk falls, aspirin’s absolute benefit shrinks, but bleeding risk does not.
This is why the USPSTF 2022 no longer recommends routine aspirin initiation for primary prevention, particularly in adults aged 60 and above, and instead supports individualized decisions for selected adults aged 40–59.
Primary prevention today is no longer pill-centric. It is risk-centric.
Tight hypertension control, appropriate statin therapy, diabetes optimization, smoking cessation, metabolic health, and early detection of atrial fibrillation prevent far more first events than blanket aspirin ever did.
Aspirin remains powerful in secondary prevention. In primary prevention, however, it has shifted from default therapy to a carefully selected exception.
Perhaps this reflects the quiet maturity of modern medicine. Good prevention is not about doing more, but about doing what matters most for the right patient at the right time.
Curious to hear from colleagues. Has aspirin prescribing for primary prevention declined in your practice?”
Stay updated with Hemostasis Today.
-
Feb 4, 2026, 16:14Kapka Miteva: Why Sex and Gender Matter in Ischemic Heart Disease
-
Feb 4, 2026, 16:11Desapriya Ediriweera: Aspirin and Cancer Prevention – Time to Update the Story
-
Feb 4, 2026, 13:42David Lloyd: Thanks Lisa Murphy for Your Leadership
-
Feb 4, 2026, 13:21Aleksandar Sič: Happy to Have 2 Abstracts Published in Stroke
-
Feb 4, 2026, 12:44Donovan Sandoval: Honored to Serve as President of Strides for Strokes
-
Feb 4, 2026, 12:34Owen McCarty: Our Recent Study on The Pathogenic Effects of Anthrax Infection
-
Feb 4, 2026, 12:16Amy Goundry: Introducing Blood and Plasma
-
Feb 4, 2026, 11:14Abdul Mannan: 216 Free Flashcards for One of the Toughest Chapters in Haematology
-
Feb 4, 2026, 11:06Eric Boilard։ How Platelets Can Promote Disease in Autoantibody-Mediated Inflammatory Conditions

