
Soroush Sohrabi: The Hidden Biology of Sclerotherapy and Mechanisms Beyond Endothelial Injury
Soroush Sohrabi, Consultant vascular and ednovascular surgeon at NMC Healthcare, shared a post on LinkedIn:
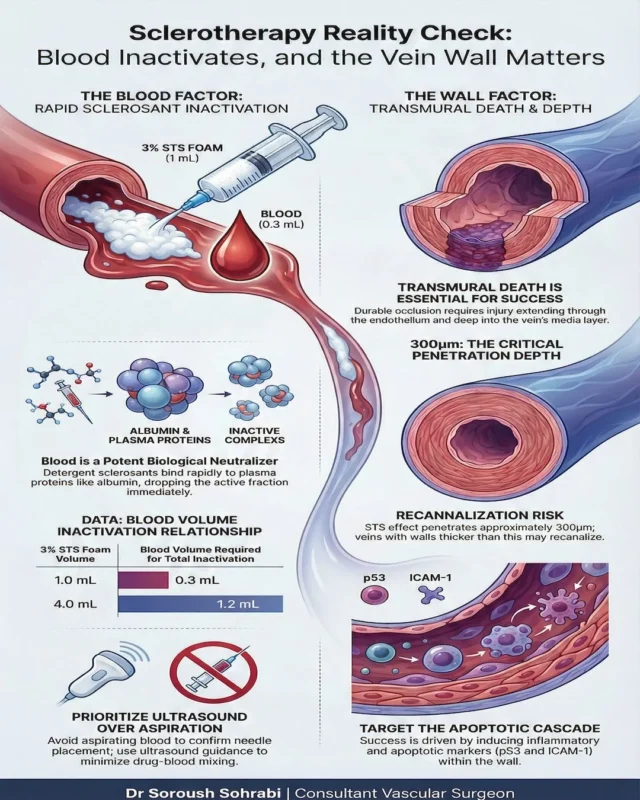
“Sclerotherapy Reality Check: Blood Inactivates — and the Vein Wall Matters
We often describe sclerotherapy in simple terms: inject the sclerosant, damage the endothelium, the vein closes.
The biology is more complex.
Two important experimental studies help clarify what is really happening:
‘Implication of foam sclerosant inactivation by human whole blood in a laboratory setting’
and
‘Media Damage Following Detergent Sclerotherapy Appears to be Secondary to the Induction of Inflammation and Apoptosis: An Immunohistochemical Study Elucidating Previous Histological Observations.’
These papers demonstrate two critical realities.
- First, blood is not passive. It actively reduces sclerosant activity. Detergent agents rapidly bind to plasma proteins such as albumin, forming inactive complexes. Even small volumes of blood can significantly decrease the active fraction available to act on the vein wall.
- Second, durable vein closure depends on more than superficial endothelial injury. Successful treatment requires deeper medial damage driven by inflammatory and apoptotic pathways. If injury remains too superficial relative to wall thickness, recanalisation becomes more likely.
In simple terms:
- Blood reduces effective drug activity
- The vein wall response determines durability
- Endothelial irritation alone is not enough
Why this matters clinically ?
These mechanistic insights help explain why outcomes vary:
- Larger veins behave differently from smaller veins
- Technique influences drug–wall contact time
- Mixing with blood reduces effective concentration
- Wall thickness influences long-term closure
- Sclerotherapy is not just a chemical injection. It is a biological interaction between sclerosant, blood, and vessel wall.
Understanding that interaction helps us refine technique, counsel patients more accurately, and improve durability of results.
What changes, if any, have these mechanisms prompted in your own approach to sclerotherapy?”
Stay updated with Hemostasis Today.
-
Feb 18, 2026, 16:23Hamad Abbasi: Why are Coronary Stents so Expensive?
-
Feb 18, 2026, 16:08Carlos Doti: AstraZeneca’s Expanding Impact in Blood Cancer Care
-
Feb 18, 2026, 16:05Shiny K. Kajal: Routine vs Massive Transfusion Protocol
-
Feb 18, 2026, 16:03Maria Farid: Successful Consultative Hematology and Transfusion Medicine Workshop at PKLI
-
Feb 18, 2026, 15:59Ella Lawson: Could Erythritol Harm the Brain’s Blood Vessels?
-
Feb 18, 2026, 15:55Amelia Carro Hevia: Defining the Future of Cardiovascular Medicine at ACC 2026
-
Feb 18, 2026, 15:47Marilena Vrana: Securing Sustainable Plasma Supply for Europe’s Growing Patient Needs
-
Feb 18, 2026, 15:28Riccardo Mazza։ Personalized Anticoagulation in Atrial Fibrillation
-
Feb 18, 2026, 15:26Beverlyn Anyango Polet: Bold Solutions for Maternal and Reproductive Health at the AYSRHR 2026

