Dr Wael El Banna/LinkedIn
Oct 5, 2025, 08:30
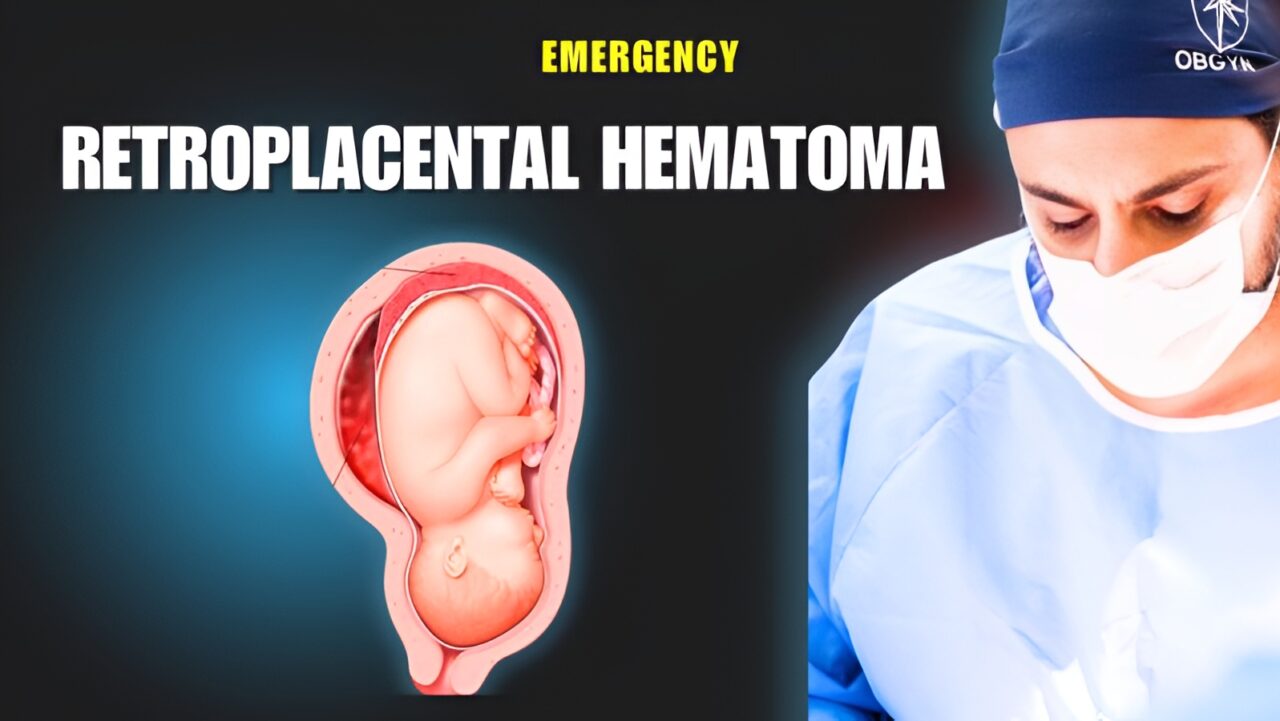
Dr Wael El Banna: How A Retroplacental Hematoma Looks Like In A Surgery Room
Dr Wael El Banna, OBGYN Consultant at FertiClinic Fertilization Group, Owner of ElBanna Group, posted on LinkedIn:
”How a retroplacental hematoma looks like in a surgery room. (watch that video )
The key management steps are :
Immediate Resuscitation and Multidisciplinary Care
- Initial focus is on maternal resuscitation following the ABC approach: airway, breathing, and circulation.
- Management should be according to locally-created massive obstetric hemorrhage protocols, led by a senior obstetrician, anesthetist, haematologist, and the midwifery team, with laboratory and portering staff alerted.
- Bloods should be immediately sent for blood grouping, crossmatch, full blood count, and coagulation screen, with 4 units of crossmatched blood prepared.
- Senior and experienced staff should be involved as early as possible in both obstetric and anaesthetic roles.
Management of Coagulopathy
- Disseminated intravascular coagulation (DIC) can develop rapidly in massive abruption; urgent clotting studies and platelet count are necessary.
- Up to 4 units of fresh frozen plasma (FFP) and 10 units of cryoprecipitate can be administered empirically if relentless bleeding persists while awaiting test results.
- Haematology input is vital for guiding further transfusions and clotting factor support.
Delivery
- If maternal or fetal compromise is evident, immediate delivery is required.
- Mode of delivery depends on fetal and maternal status:
- If fetal death has occurred and maternal condition is stable, vaginal delivery is generally recommended.
- If fetus is alive but compromised, expedite delivery by caesarean section, unless vaginal delivery is imminent.
Additional Considerations
- Continuous maternal and fetal monitoring is essential during and after the acute event.
- All RhD-negative women should receive anti-D immunoglobulin if more than 20 weeks gestation.
- Ongoing monitoring for PPH, renal dysfunction, and further coagulopathy is needed post-delivery.
- If the patient develops hypovolemia or shock, ICU-level support and ongoing multidisciplinary care are mandatory.”
Stay updated with Hemostasis Today.
-
Mar 1, 2026, 13:17Michael Makris։ Extraterrestrial Regolith as a Trigger of the Intrinsic Coagulation Pathway
-
Mar 1, 2026, 13:11Strategic Planning Day to Shape The Future of Thrombosis and Haemostasis – THANZ
-
Mar 1, 2026, 13:06Simon Senanu: Not Every Thrombocytopenia Is Real
-
Mar 1, 2026, 12:53Kevin Tang: Evolving Burden of CVD Across Asia and Its Broader Implications for Global Health Policy
-
Mar 1, 2026, 12:02Hassan Raza: Building Sustainable Support for People with Bleeding Disorders in Pakistan
-
Mar 1, 2026, 11:40Naradja Wissmar: Raised IL-32 as a Hint to Long-Term Immune Activation Post-COVID
-
Mar 1, 2026, 11:10Mehran Ghasemzadeh: A Novel Panel Bridging Platelet Function and Clinical Presentation in Chronic ITP
-
Mar 1, 2026, 10:47Tagreed Alkaltham: In Transfusion Medicine, Every Reaction Deserves An Answer
-
Mar 1, 2026, 10:31Deborah Siegal Explores ARTESiA in The CLOT Conversation’s Latest Episode

