
Seyed Mohsen Jahromi Moghadam: Antithrombotic Therapy After Transcatheter Structural Heart Interventions
Seyed Mohsen Jahromi Moghadam, Advanced Interventional Cardiologist at Razavi Hospital, posted on LinkedIn:
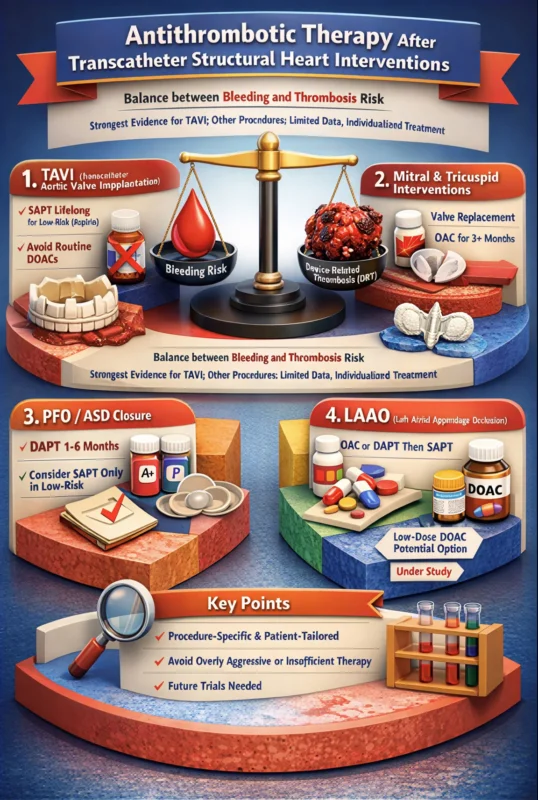
”After transcatheter structural heart interventions, antithrombotic therapy must balance prevention of device-related thrombosis (DRT) against bleeding risk. Evidence is strongest for TAVI; for other procedures, data are limited and treatment should be individualized.
1) Transcatheter Aortic Valve Implantation (TAVI)
Patients without an indication for oral anticoagulation (OAC):
• Lifelong single antiplatelet therapy (SAPT), usually low-dose aspirin, is recommended.
• Dual antiplatelet therapy (DAPT) increases bleeding without ischemic benefit.
• Routine DOAC use is discouraged due to higher mortality and bleeding despite reducing subclinical leaflet thrombosis (SLT).
Subclinical leaflet thrombosis (HALT/RLM):
• More frequent with antiplatelet therapy than with OAC.
• Associated with higher stroke/TIA risk.
• Temporary OAC (VKA or DOAC) for ~3–6 months is recommended when SLT is detected, with CT follow-up.
Patients with an indication for chronic OAC (e.g., atrial fibrillation):
• OAC alone is preferred.
• Adding antiplatelet therapy increases bleeding without benefit.
• DOACs appear reasonable alternatives to VKAs if appropriately dosed and without routine antiplatelet use.
2) Mitral and Tricuspid Interventions
• Valve replacement (TMVI/TTVI): High risk of DRT → OAC for at least 3 months is generally recommended.
• Edge-to-edge repair (TEER): DRT is rare; resume OAC if indicated or use short-term SAPT.
• Evidence comparing DOACs vs VKAs is limited, but DOACs may reduce bleeding.
3) Patent Foramen Ovale (PFO) / Atrial Septal Defect (ASD) Closure
• Traditional approach: DAPT for 1–6 months, then SAPT.
• Recent observational data suggest no clear advantage of DAPT over SAPT.
• In selected low-risk patients, complete discontinuation of antithrombotic therapy after endothelialization may be safe, but evidence is still evolving.
4) Left Atrial Appendage Occlusion (LAAO)
• DRT occurs in <5%, mostly within the first 90 days, but markedly increases stroke risk.
• Regimens vary:
• Short-term OAC or DAPT followed by SAPT is common.
• Emerging evidence suggests low-dose or half-dose DOAC monotherapy may reduce both DRT and bleeding in high-bleeding-risk patients.
• Optimal regimen remains under investigation in ongoing RCTs.
Conclusion
• Antithrombotic strategies after transcatheter structural heart interventions must be procedure-specific and patient-tailored.
• Overly aggressive therapy increases bleeding, while insufficient therapy increases thrombotic risk.
• Future trials (including imaging-guided and factor XIa inhibitor strategies) aim to refine this balance.”
Stay updated with Hemostasis Today.
-
Feb 2, 2026, 16:45Shashank Joshi: Switching Among Oral Anticoagulants
-
Feb 2, 2026, 16:40Zeinab Mubarak: How do Women Benefit from Menstrual Blood?
-
Feb 2, 2026, 16:23Ignacio Diaz Lorenzo: Reflecting on the Management of Acute Pulmonary Embolism
-
Feb 2, 2026, 16:18Tareq Abadl: Persistent Anti-β2GPI IgG Is Not a Coincidence – It’s Pathology
-
Feb 2, 2026, 16:06Christian Heiss։ When Diabetes and PAD Overlap, Cardiovascular and Limb Risks Rise
-
Feb 2, 2026, 16:02Shiny K. Kajal: Platelet Transfusion Is a Therapy – Not a Reflex
-
Feb 2, 2026, 15:37Rana Saifi: An Exciting Time for the Bleeding Disorders Community
-
Feb 2, 2026, 13:08Hammam Alminshawi: Time is Brain – Optimizing MRI for Acute Ischemic Stroke
-
Feb 2, 2026, 12:53Lucie Gelon: Proud to Share My 1st Achievements in The Scientific and Platelet World

