
Arun V J: Do You Know What SDP or Apheresis Platelet Is?
Arun V J, The Leader of Transfusion Medicine at Malabar Medical College, shared on LinkedIn:
”Do You Know What SDP or Apheresis Platelet Is?
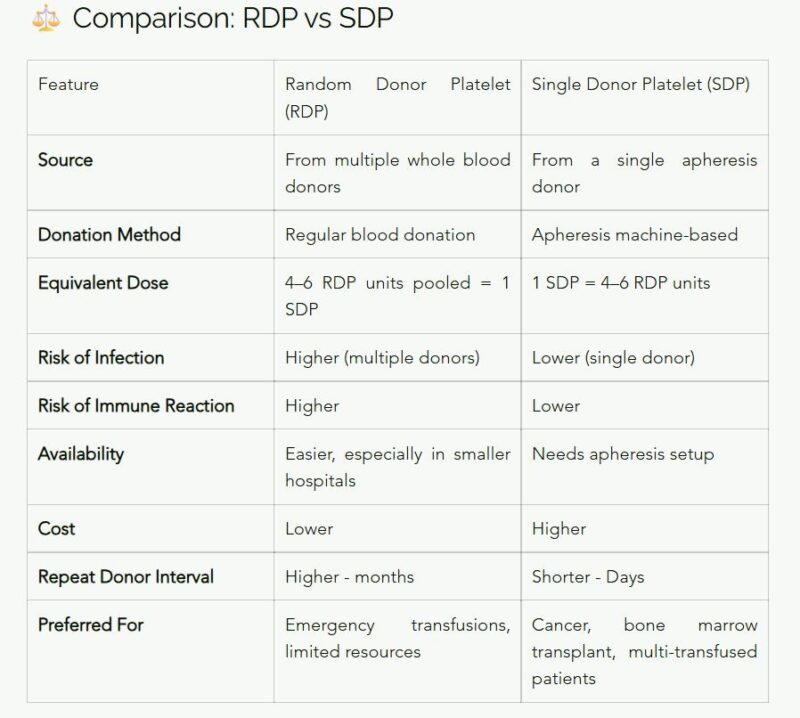
Most doctors, donors, and even healthcare workers don’t truly understand what an SDP is — or how it’s different from an RDP.
Because when we misunderstand science, patients pay the price.
First, what are we talking about?
RDP (Random Donor Platelet):
Platelets separated from whole blood donations.
A single unit gives a small platelet yield.
So, for one patient, you usually pool platelets from 4–6 different donors to reach the required dose.
SDP (Single Donor Platelet):
Collected through apheresis, where a machine selectively removes platelets and returns the rest of your blood.
One SDP = 4–6 RDPs in platelet count — but from one donor only.
Why this matters
- When a patient receives RDPs, they’re exposed to multiple immune systems.
- Each donor’s platelets have different antigens.
- This increases risks like immune reactions and platelet refractoriness (when the patient stops responding to transfusions).
- SDP minimizes this risk.
That’s why it’s preferred for cancer patients, bone marrow transplants, and those needing repeated transfusions — not for “faster rise.”
Why SDP Costs More
- It’s not “premium blood.”
- The cost includes sterile single-use kits, apheresis machine use, longer donation time, and trained personnel.
- But it gives safer platelets, traceable donors, and fewer complications.
Common Myths (Let’s Bust Them)
Myth 1: “SDP gives faster platelet count rise.”
False. Rise depends on the patient’s body, not platelet type.
Myth 2: “SDP is only for rich people.”
False. Many hospitals subsidize or cover it under insurance.
Myth 3: “SDP donation is painful.”
False. It’s smooth, safe, and you get your red cells back.
The Bigger Picture
- In developed countries, apheresis platelets are the standard.
- In India and similar regions, we’re still transitioning — mainly because of awareness gaps & cost of technology.
- If every doctor and donor understood the difference, we’d save time, cost, and lives.
The Third Thinker Takeaway
- Blood donation isn’t just kindness.
- It’s applied science.
- Every time you donate — or prescribe — you shape someone’s tomorrow.
Because better understanding leads to better care.
Read the detailed version here.
If you learned something new, drop a or share it — more awareness means fewer misconceptions, and more lives saved.”
Stay updated with Hemostasis Today.
-
Feb 22, 2026, 14:16Ilenia Calcaterra: From Representation to Intellectual Independence in Women in Science
-
Feb 22, 2026, 13:27Pete Stibbs: New AHA and ACC PE Guidelines Finally Align with Real Clinical Practice
-
Feb 22, 2026, 10:39Tagreed Alkaltham: Fibrinogen Concentrate Is a Deliberate Clinical Choice in Acute Bleeding
-
Feb 22, 2026, 09:38Abdulrahman Nasiri: Significant Shifts In The 2026 AHA/ACC Guidelines for Acute Pulmonary Embolism
-
Feb 22, 2026, 09:22Shiny K. Kajal: Not All Transfusion Reactions Are Immunohematologic Incompatibilities
-
Feb 22, 2026, 09:12Arun V J։ The Hidden Risks in Every Blood Bag
-
Feb 22, 2026, 08:56Parandzem Khachatryan։ How Hard Is It to Be a Mom, a Wife, a Professor, and a Doctor All at Once?
-
Feb 22, 2026, 08:46Anirban Sen Gupta Presents Bioinspired Platelet Surrogates at MTEC
-
Feb 22, 2026, 08:31Heghine Khachatryan: Advancing Care for Women and Girls with Bleeding Disorders is A Matter of Equity

