
Samwel Mikaye Explains Blood Components and Their Clinical Use
Samwel Mikaye, CEO of SaMik Medical Center, posted on LinkedIn:
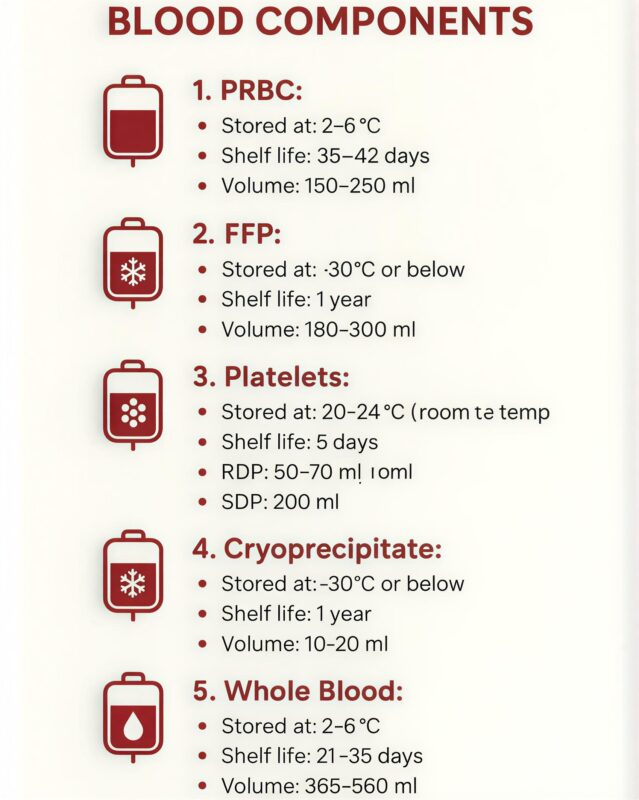
”BLOOD COMPONENTS
Blood can be separated into individual components to allow targeted therapy, reduce volume overload, and preserve valuable resources.
1. Whole Blood
• Composition: RBCs, plasma, platelets, clotting factors.
• Use: Rarely used today; mainly in massive hemorrhage where both RBCs and plasma are needed.
• Volume: ~450–500 mL per unit.
2. Red Blood Cells (RBCs) / Packed Red Cells
• Composition: Concentrated RBCs, most plasma removed.
• Indications:
• Symptomatic anemia
• Acute blood loss
• Hemoglobin <7–8 g/dL in stable patients
• Goal: Improve oxygen-carrying capacity.
• Volume: ~250–300 mL per unit.
• Key point: One unit increases Hb by ~1 g/dL in adults.
3. Platelet Concentrates
• Composition: Platelets, some plasma.
• Indications:
• Thrombocytopenia (<10,000/µL without bleeding)
• Active bleeding with low platelets
• Pre-surgery prophylaxis if platelets <50,000/µL
• Forms: Random donor platelets, apheresis platelets.
• Volume: ~50 mL per random donor unit; ~200–300 mL per apheresis unit.
4. Fresh Frozen Plasma (FFP)
• Composition: All clotting factors, plasma proteins.
• Indications:
• Coagulation factor deficiencies (e.g., liver disease, DIC)
• Massive transfusion protocols
• Warfarin reversal (if urgent)
• Volume: 200–250 mL per unit
• Storage: Frozen; thaw before use.
5. Cryoprecipitate
• Composition: Concentrated clotting factors (Factor VIII, fibrinogen, vWF, Factor XIII).
• Indications:
• Hypofibrinogenemia (<100 mg/dL)
• Hemophilia A (if factor concentrates unavailable)
• Massive bleeding with low fibrinogen
• Volume: ~10–20 mL per unit
6. Granulocyte/White Cell Concentrates
• Composition: Concentrated WBCs
• Indications: Rare; for severe neutropenia with infection unresponsive to antibiotics.
• Key point: Limited availability, short shelf-life.
General Principles
• Cross-matching: Required for RBCs and whole blood.
• Compatibility:
• O-negative → universal donor for RBCs.
• AB plasma → universal donor plasma.
• Storage:
• RBCs: 1–6°C, up to 35–42 days depending on anticoagulant.
• Platelets: 20–24°C, constant agitation, 5 days.
• FFP/Cryoprecipitate: −18°C or lower, up to 1 year.
Key Takeaways
1. Blood components allow targeted therapy instead of whole blood.
2. Correct selection depends on deficient element: RBCs → anemia, platelets → thrombocytopenia, plasma → clotting factors.
3. Always monitor patient response and transfusion reactions.”
Stay informed with Hemostasis Today.
-
Feb 22, 2026, 14:16Ilenia Calcaterra: From Representation to Intellectual Independence in Women in Science
-
Feb 22, 2026, 13:27Pete Stibbs: New AHA and ACC PE Guidelines Finally Align with Real Clinical Practice
-
Feb 22, 2026, 10:39Tagreed Alkaltham: Fibrinogen Concentrate Is a Deliberate Clinical Choice in Acute Bleeding
-
Feb 22, 2026, 09:38Abdulrahman Nasiri: Significant Shifts In The 2026 AHA/ACC Guidelines for Acute Pulmonary Embolism
-
Feb 22, 2026, 09:22Shiny K. Kajal: Not All Transfusion Reactions Are Immunohematologic Incompatibilities
-
Feb 22, 2026, 09:12Arun V J։ The Hidden Risks in Every Blood Bag
-
Feb 22, 2026, 08:56Parandzem Khachatryan։ How Hard Is It to Be a Mom, a Wife, a Professor, and a Doctor All at Once?
-
Feb 22, 2026, 08:46Anirban Sen Gupta Presents Bioinspired Platelet Surrogates at MTEC
-
Feb 22, 2026, 08:31Heghine Khachatryan: Advancing Care for Women and Girls with Bleeding Disorders is A Matter of Equity

