
Dr Abdul Mannan: What’s Your Approach to Diagnosing Iron Deficiency in Tricky Cases?
Dr Abdul Mannan, Consultant Haematologist at Betsi Cadwaladr University Health Board, posted on LinkedIn:
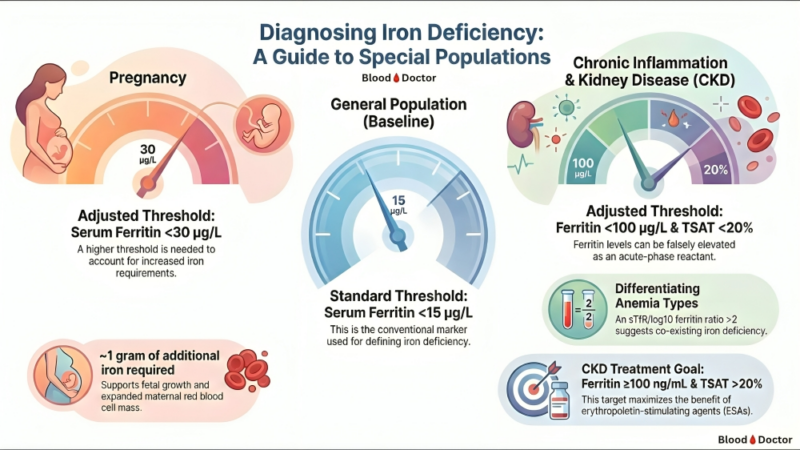
“After years of managing anaemia across different patient populations, I’ve learned one thing: that single ferritin number on your screen? It’s not telling you the whole truth.
Let me explain with three patients I see regularly.
Patient 1: The “Normal” Pregnant WomanHer ferritin comes back at 20 µg/L.
“Normal range,” says the lab slip.
But here’s what the lab doesn’t know: she’s growing a human being. That baby needs iron. Her expanding blood volume needs iron. We’re talking about 1 gram of additional iron over 9 months.
A ferritin of 20 in pregnancy? That’s not normal. That’s a deficiency waiting to cause problems.
The fix: In pregnancy, think <30 µg/L as your red flag.
Patient 2: The CKD Patient with “Adequate” Iron
Ferritin: 85 µg/L.
Looks fine, right?
Wrong.
This patient has chronic kidney disease. Inflammation. Ferritin is an acute phase reactant — it rises when the body is inflamed, regardless of actual iron stores.
I’ve seen CKD patients with ferritin of 200 who were profoundly iron deficient.
The fix: In CKD and inflammation, you need TWO numbers: → Ferritin <100 µg/L AND → Transferrin saturation <20%
Both. Not one. Both.
And when you’re really stuck? The sTfR/log10 ferritin ratio >2 points toward true iron deficiency hiding behind inflammation.
Patient 3: The Textbook Case
Healthy adult. No inflammation. No pregnancy.
Ferritin <15 µg/L = iron deficiency.
Simple. Clean. The one time ferritin actually behaves.
The Bottom Line:
One number. Three completely different interpretations depending on who’s sitting in front of you.
Medicine isn’t about memorizing reference ranges. It’s about knowing when those ranges don’t apply.
The best doctors I know don’t just read results. They read context.
Quick Reference:
General population: Ferritin <15 µg/L
Pregnancy: Ferritin <30 µg/L
CKD/Inflammation: Ferritin <100 µg/L + TSAT <20%
Save this. Share it. Your patients will thank you.
What’s your approach to diagnosing iron deficiency in tricky cases?”
Follow the latest with Hemostasis Today.
-
Jan 31, 2026, 16:35IV Thrombolysis Does Not Improve Vision in Acute CRAO: Ahmed Koriesh on TenCRAOS Study
-
Jan 31, 2026, 16:24Joyce John Chalakkal: The Dangerous Area of The Face….
-
Jan 31, 2026, 16:04Rayya Saadiq Reflects On Qatar Health Congress 2026
-
Jan 31, 2026, 15:12Amar Raval on Oral Thin Film Drug Delivery Systems for Thrombosis Therapy
-
Jan 31, 2026, 14:40Heghine Khachatryan on WFH’s Call to Advance Health Equity for People with Bleeding Disorders
-
Jan 31, 2026, 14:10Emilia Arturo: Snake Venom, Clotting, and CryoEM!
-
Jan 31, 2026, 08:13Ming Y Lim On The Value of National Mentorship
-
Jan 31, 2026, 06:37Christian Schulze Presents The Post-Hoc Analysis of the DanGer Shock Trial
-
Jan 31, 2026, 06:27Negative Trials Matter: Anne Hege Aamodt Shares The TenCRAOS Trial

