
Tarek Abbas: Patients With Advanced Cardiovascular Kidney Metabolic Syndrome Have High Risk of Cardiovascular Complications
Tarek Abbas, Senior Consultant of Nephrology and Renal Transplantation at Mansoura University School of Medicine, shared a post on LinkedIn:
“What to do with key cardiovascular drugs when kidney function worsens?
Title: What to do with key cardiovascular drugs when kidney function worsens?
Authors: Karin Bergen, Jonas Spaak
Read full study here.
Clinical Kidney Journal, sfaf354,
Published: 21 November 2025
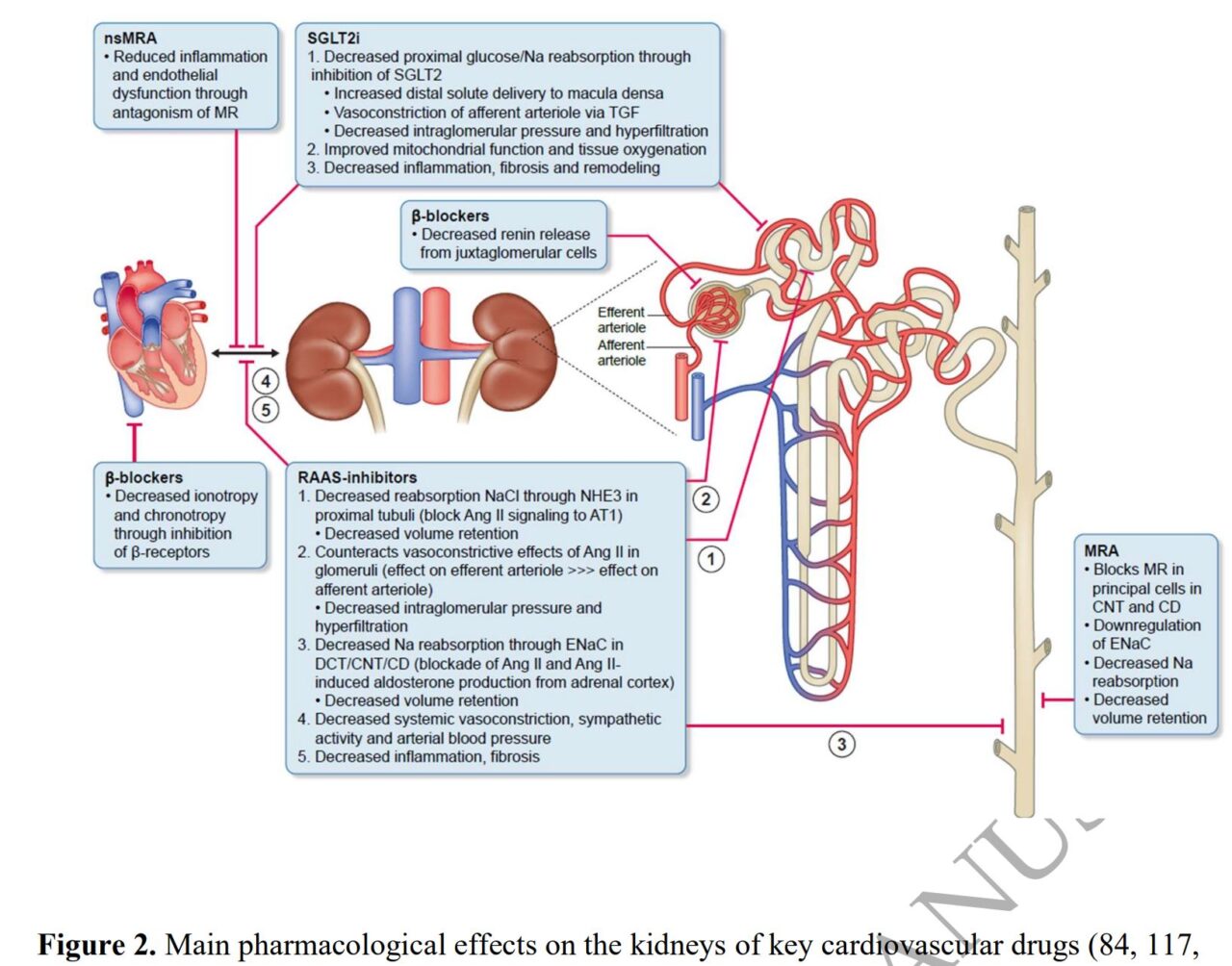
Patients with advanced cardiovascular kidney metabolic syndrome have high risk of cardiovascular complications.
Guideline-directed medical therapies (GDMT) are critical for mitigating cardiovascular risk and improving prognosis.
Patients with more advanced kidney disease have frequently been excluded from the foundational cardiovascular outcome trials, leaving clinicians with a paucity of evidence with regards to the cardiovascular benefits and potential risks involved in initiating or maintaining GDMT for cardiovascular diseases in patients with chronic kidney disease stages 4 and 5.
Systematic underutilization of GDMT among patients with advanced chronic kidney disease (CKD) is caused by a combination of clinical inertia and a legitimate fear of potential side-effects such as hyperkalemia and rises in creatinine, which necessitate repeat lab monitoring, dose adjustment and additional potassium lowering treatment.
In this clinical review, the authors summarized the accumulating evidence of using key cardiovascular drugs among patients with advanced CKD, (with an emphasis on GDMT in patients with heart failure), and outlined the treatment approach used in integrated heart-nephrology-diabetes clinic.
Since the evidence is not clear and patients are older, frailer and have more multimorbidity than those included in clinical trials, sound clinical judgment, individual patient tolerability as well as shared decision making are key.
Continuous alignment treatment goals with patient preferences across different phases of life and adjusting GDMT in the face of increasing frailty.”
Stay updated with Hemostasis Today.
-
Feb 25, 2026, 16:47Alan Nurden: Platelet Defects Explain Bleeding in EHDS Patients
-
Feb 25, 2026, 16:40Mohammed Almohammadi: Uniting Leaders in Laboratory Hematology at the 1st Saudi ISLH Joint Conference
-
Feb 25, 2026, 16:37Salihu Asimawu: Inflammation Is Not a Disease – Hats Off to the Heroes Inside Us
-
Feb 25, 2026, 16:34Michael Makris: Biomarin Has Decided to Withdraw Roctavian from the Market
-
Feb 25, 2026, 16:25Tagreed Alkaltham: The Blood Banker Personality
-
Feb 25, 2026, 16:17Sanjay Ahuja: Insightful Talk on 100 Years of VWD by Jorge Di Paola
-
Feb 25, 2026, 15:20Michael Shapiro։ Creating Real Pathways for Trainees in Preventive Cardiology
-
Feb 25, 2026, 15:15Ajay Kumar: Plasma Component Quality Control Standards
-
Feb 25, 2026, 15:09Wolfgang Miesbach: Efficacy, Safety and Thrombosis Signals in Haemophilia A/B with Inhibitors

