
Tareq Abadl: CMV and Transfusion – Leukoreduction vs CMV-Seronegative
Tareq Abadl, Medical Laboratory Specialist and Director of the Blood Bank at Dr. Abdelkader Al-Mutawakkil Hospital, shared a post on LinkedIn:
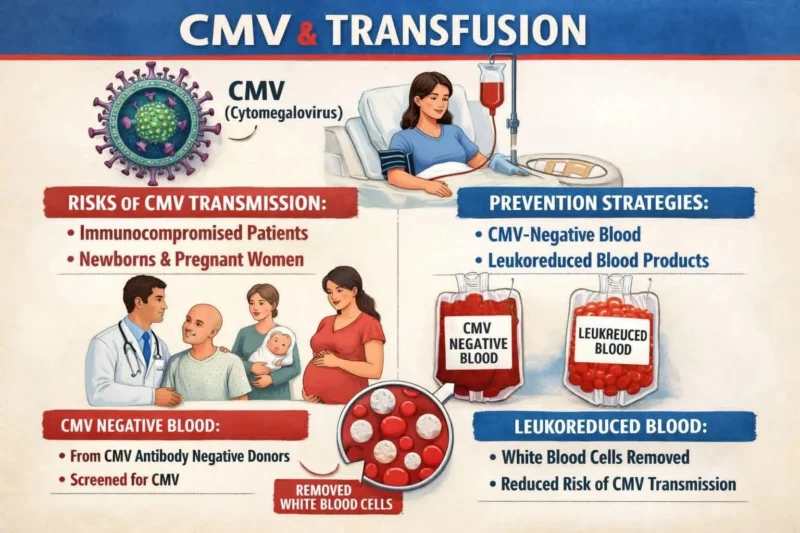
“CMV and Transfusion — Leukoreduction vs CMV-Seronegative
Cytomegalovirus (CMV) can be transmitted through blood components, but modern transfusion practice has reduced this risk dramatically.
For most at-risk patients, pre-storage leukoreduced (‘CMV-safe’) components are considered an effective alternative to routinely using CMV-seronegative units — with a few important exceptions.
What Major Authorities Say?
Organizations such as the AABB, the Centers for Disease Control and Prevention (CDC), and national blood services like Canadian Blood Services recognize that:
- Pre-storage leukoreduction significantly reduces transfusion-transmitted CMV (TT-CMV).
- Many programs consider leukoreduced (CMV-safe) and CMV-seronegative components clinically equivalent for most indications.
Important Exceptions
Maximal prevention is still recommended in certain high-risk settings:
- Intrauterine transfusion (IUT)
- Some extremely low-birthweight neonates
Selected transplant or severely immunocompromised patients (based on local policy)
- In these cases, request CMV-seronegative units in addition to leukoreduction.
- Always follow your institution’s policy and consult neonatology/transplant teams when needed.
Practical Blood Bank Guidance
Default practice:
Provide pre-storage leukoreduced components for routine transfusion.
For listed exceptions:
Request CMV-seronegative units plus leukoreduction.
Document the clinical indication clearly in the order.
System optimization:
Tag ‘CMV-safe’ components automatically in the LIS.
Add a required checkbox for ‘CMV-seronegative requested’ with documented reason.
Audit compliance and outcomes periodically.
Why Leukoreduction Works?
CMV resides mainly in white blood cells.
Leukoreduction removes the majority of this cellular reservoir, dramatically lowering TT-CMV risk.
That’s why many blood services shifted away from maintaining large universal seronegative inventories — it simplifies logistics while remaining protective for most patients.
Summary
- Leukoreduction: effective protection for most patients
- CMV-seronegative units: reserved for specific high-risk scenarios
- Always align practice with local policy and patient risk profile
Modern transfusion medicine balances safety, practicality, and evidence — not tradition.”
Find more posts featuring Tareq Abadl on Hemostasis Today.
-
Feb 18, 2026, 16:24Soroush Sohrabi: The Hidden Biology of Sclerotherapy and Mechanisms Beyond Endothelial Injury
-
Feb 18, 2026, 16:23Hamad Abbasi: Why are Coronary Stents so Expensive?
-
Feb 18, 2026, 16:08Carlos Doti: AstraZeneca’s Expanding Impact in Blood Cancer Care
-
Feb 18, 2026, 16:05Shiny K. Kajal: Routine vs Massive Transfusion Protocol
-
Feb 18, 2026, 16:03Maria Farid: Successful Consultative Hematology and Transfusion Medicine Workshop at PKLI
-
Feb 18, 2026, 15:59Ella Lawson: Could Erythritol Harm the Brain’s Blood Vessels?
-
Feb 18, 2026, 15:55Amelia Carro Hevia: Defining the Future of Cardiovascular Medicine at ACC 2026
-
Feb 18, 2026, 15:47Marilena Vrana: Securing Sustainable Plasma Supply for Europe’s Growing Patient Needs
-
Feb 18, 2026, 15:28Riccardo Mazza։ Personalized Anticoagulation in Atrial Fibrillation

