
Tareq Abadl: Heparin vs Warfarin
Tareq Abadl, Medical Laboratory Specialist and Director of the Blood Bank at Dr. Abdelkader Al-Mutawakkil Hospital, shared a post on LinkedIn:
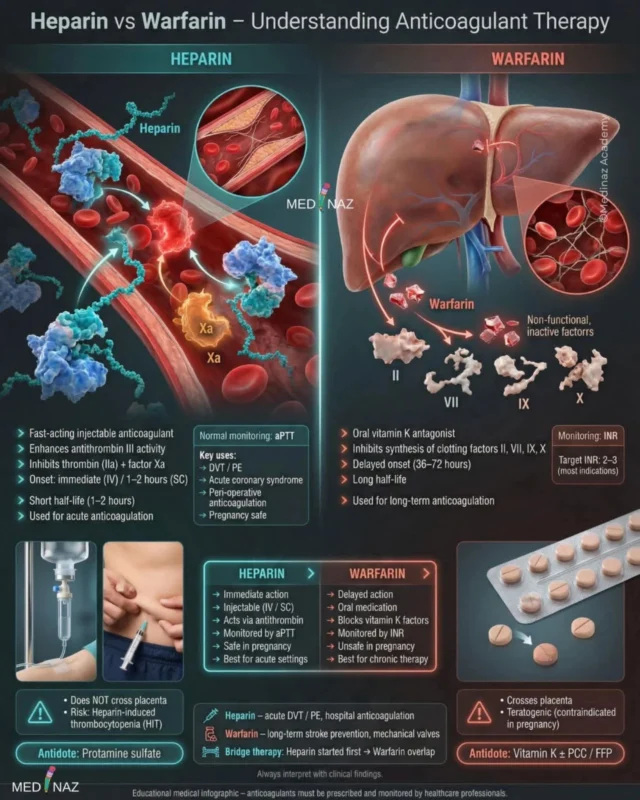
“Heparin vs Warfarin – Anticoagulant Therapy.
Both Heparin and Warfarin are blood thinners used to prevent or treat clots, but they differ greatly in mechanism, onset, route, monitoring, and safety.
HEPARIN
- What it is
• Fast-acting injectable anticoagulant
- Mechanism of action
• Enhances Antithrombin III
• Inhibits Thrombin (Factor IIa) and Factor Xa
(• Result: immediate prevention of clot extension)
• Onset and duration
• IV: immediate
• Subcutaneous: 1–2 hours
• Short half-life (~1–2 hours)
- Route
• IV or Subcutaneous
- Monitoring
• aPTT
• Main uses
• Acute DVT / PE
• Acute coronary syndromes
• Peri-operative anticoagulation
• Bridging to warfarin
• Safe anticoagulation in pregnancy
- Important points
• Does NOT cross placenta
• Preferred in pregnancy
• Used mainly for acute settings
- Major adverse effects
• Bleeding
• Heparin-Induced Thrombocytopenia (HIT)
• Osteoporosis (long-term use)
- Antidote
• Protamine sulfate
WARFARIN
- What it is
• Oral anticoagulant
• Vitamin K antagonist
- Mechanism of action
• Inhibits Vitamin K epoxide reductase
• Decreases synthesis of clotting factors: II, VII, IX, X
• Also reduces Protein C & Protein S initially
(• Result: delayed anticoagulant effect)
- Onset
• 36–72 hours (delayed)
- Route
• Oral
- Monitoring
• INR
Target INR usually 2–3
- Main uses
• Long-term anticoagulation
• Atrial fibrillation
• Mechanical heart valves
• Chronic DVT / PE prevention
• Stroke prevention
- Important points
• Crosses placenta
• Teratogenic
• Contraindicated in pregnancy
• Requires frequent INR monitoring
• Many food & drug interactions
- Major adverse effects
• Bleeding
• Skin necrosis (early due to Protein C depletion)
• Purple toe syndrome
• Fetal warfarin syndrome (if used in pregnancy)
- Antidote
• Vitamin K
• PCC or FFP for severe bleeding
Key Differences (Exam Favorite)
Heparin
- Immediate action
- Injectable
- Acts via Antithrombin III
- Monitored by aPTT
- Safe in pregnancy
- Short half-life
- Used for acute cases
Warfarin
- Delayed action
- Oral
- Blocks vitamin K factors
- Monitored by PT / INR
- Unsafe in pregnancy
- Long half-life
- Used for chronic therapy
Bridging Therapy (Very Important)
- Heparin is started first
- Warfarin added simultaneously
- Heparin stopped only after INR becomes therapeutic
Reason:
Warfarin initially reduces Protein C to temporary hypercoagulable state
Relationship Between Heparin and Warfarin and Coagulation Tests (PT and aPTT)
Heparin primarily affects the Intrinsic pathway by enhancing Antithrombin III and inhibiting Thrombin and Factor Xa.
• This leads to prolongation of aPTT.
• PT is usually normal.
Warfarin primarily affects the Extrinsic pathway, especially Factor VII, by inhibiting vitamin K–dependent clotting factor synthesis.
• This leads to prolongation of PT and elevation of INR.
• aPTT is usually normal or only mildly prolonged.
High-yield exam rule:
Heparin to aPTT
Warfarin to PT / INR”
More posts from Tareq Abadl on Hemostasis Today.
-
Feb 2, 2026, 17:07Mary Cushman: New Research on Aspirin Use in Pregnancy and Stroke Risk in Offspring
-
Feb 2, 2026, 16:52Aravind Palraj: Young Stroke is Never Just Stroke
-
Feb 2, 2026, 16:48Seyed Mohsen Jahromi Moghadam: Antithrombotic Therapy After Transcatheter Structural Heart Interventions
-
Feb 2, 2026, 16:45Shashank Joshi: Switching Among Oral Anticoagulants
-
Feb 2, 2026, 16:40Zeinab Mubarak: How do Women Benefit from Menstrual Blood?
-
Feb 2, 2026, 16:23Ignacio Diaz Lorenzo: Reflecting on the Management of Acute Pulmonary Embolism
-
Feb 2, 2026, 16:18Tareq Abadl: Persistent Anti-β2GPI IgG Is Not a Coincidence – It’s Pathology
-
Feb 2, 2026, 16:06Christian Heiss։ When Diabetes and PAD Overlap, Cardiovascular and Limb Risks Rise
-
Feb 2, 2026, 16:02Shiny K. Kajal: Platelet Transfusion Is a Therapy – Not a Reflex

