
Mohamed Magdy Badr: Post-Thrombotic Limb and Venous Ulcer Healing
Mohamed Magdy Badr, Wound Care Consultant at Armed Force Rehabilitation Center, posted on LinkedIn:
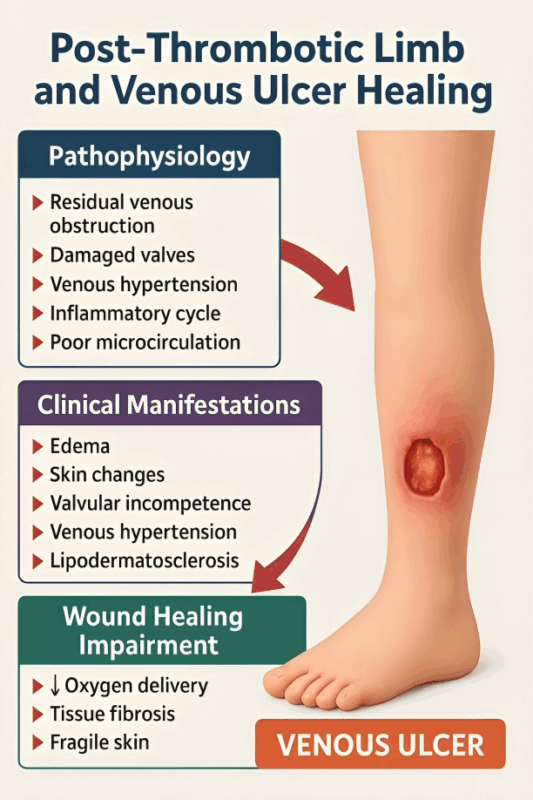
”Post-Thrombotic Limb and Venous Ulcer Healing: Why These Wounds Are So Difficult – and How We Can Improve Outcomes
Post-Thrombotic Syndrome (PTS) remains one of the most challenging etiologies behind chronic venous ulcers.
After a DVT, many patients develop residual venous obstruction, valvular incompetence, venous hypertension, edema, skin changes, and microcirculatory failure — all of which create a hostile environment for wound healing.
1. Pathophysiology: Why PTS Delays Healing
- Residual venous obstruction → impaired blood return
- Damaged valves → severe reflux
- Venous hypertension → capillary leakage, edema
- Inflammatory cycle → leukocyte trapping, tissue fibrosis
- Poor microcirculation → ↓ oxygen delivery and nutrient supply
- Lipodermatosclerosis → chronic skin fibrosis and fragility
Together, these factors make PTS-related venous ulcers slower to heal and more prone to recurrence.
2. Clinical Challenges in Healing
- Hard, brawny edema resistant to basic compression
- Fibrotic skin with poor elasticity
- Recurrent cellulitis
- Mixed etiology (venous + lymphedema, obesity, CKD, heart failure)
- Poor adherence to long-term compression
- Delayed diagnosis of iliac obstruction (common in PTS)
3. Principles of Effective Management
A. Venous Outflow Restoration (When Needed)
- Consider iliac vein duplex / IVUS in non-healing or recurrent ulcers
- Address residual iliac/femoral obstruction
- Stenting when indicated improves healing and reduces recurrence
B. Compression Therapy (The Cornerstone)
- Multilayer bandaging (40–60 mmHg at ankle)
- Short-stretch or zinc paste boots in severe edema
- Velcro wraps for obese or non-compliant patients
- Long-term maintenance stockings after closure
C. Edema and Inflammation Control
- Limb elevation
- Manual lymphatic drainage when mixed disease
- Anti-inflammatory compression (Unna boot) in lipodermatosclerosis
D. Wound Bed Optimization
- Aggressive debridement of fibrin/tissue necrosis
- Moisture-balanced dressings
- Address biofilm (regular sharp debridement + HOCl)
- Consider advanced therapies: NPWT, biological dressings, PRP
E. Risk Factor Modification
- Weight reduction
- Glycemic control
- Treat heart/renal dysfunction
- Encourage mobility and calf pump activity
4. The Reality: Healing Takes Time
- PTS-related ulcers heal slower than typical venous ulcers
- Recurrence is high without lifelong compression
- Early detection of venous obstruction is critical
- Multidisciplinary care significantly improves outcomes
Take-Home Message
- Post-thrombotic venous ulcers represent the intersection of obstruction, reflux, edema, and microvascular failure.
- Healing requires restoring venous outflow, strict compression, edema reduction, wound bed optimization, and long-term maintenance therapy.
- These wounds can heal – but only with structured, aggressive, and comprehensive venous management.”
Stay informed with Hemostasis Today.
-
Mar 1, 2026, 05:44Ilenia Calcaterra: Innovation In Rare Diseases Is Never Abstract
-
Feb 28, 2026, 17:03Investing in Education, Prevention, and Lifesaving Research for a Healthier Tomorrow – AHA
-
Feb 28, 2026, 17:00Pamela Gavin: 1 in 10 Americans Live With A Rare Disease – That Is Not Rare, That Is Public Health
-
Feb 28, 2026, 16:59Thomas Rocco Jr: Exploring Agentic AI in Cardiovascular Medicine
-
Feb 28, 2026, 16:50Rob Maloney: Normalcy Is Not A Small Thing In Rare Disease
-
Feb 28, 2026, 16:49Céline Chapelle: Evaluating 6-Month Risks of Recurrent VTE and Major Bleeding With Tinzaparin
-
Feb 28, 2026, 16:46Nicolas Hulscher: Nattokinase Dissolves 84% of Amyloid Microclots In Vitro
-
Feb 28, 2026, 16:46Alfonso Tafur: Preventing Post-Hospitalization Blood Clots Using Precision Tools and Systems
-
Feb 28, 2026, 16:39Anel Karisik: Do Antidepressants Influence Swallowing Recovery After Acute Ischemic Stroke?

