
Dr Abdul Mannan: The Molecular “Switch” That Saves Lives – Pathophysiological Review of the Protein C System
Dr Abdul Mannan, Consultant Haematologist at Betsi Cadwaladr University Health Board, shared a post on LinkedIn:
“The Molecular “Switch” That Saves Lives: A Pathophysiological Review of the Protein C System
In the world of clinical haematology, balance is a survival mechanism. Today, we are analyzing the Systemic Dysregulation of the Protein C System—a catastrophic failure that leads to the medical emergency of Purpura Fulminans (PF).
Part 1: The Physiological Masterpiece (The Normal State)
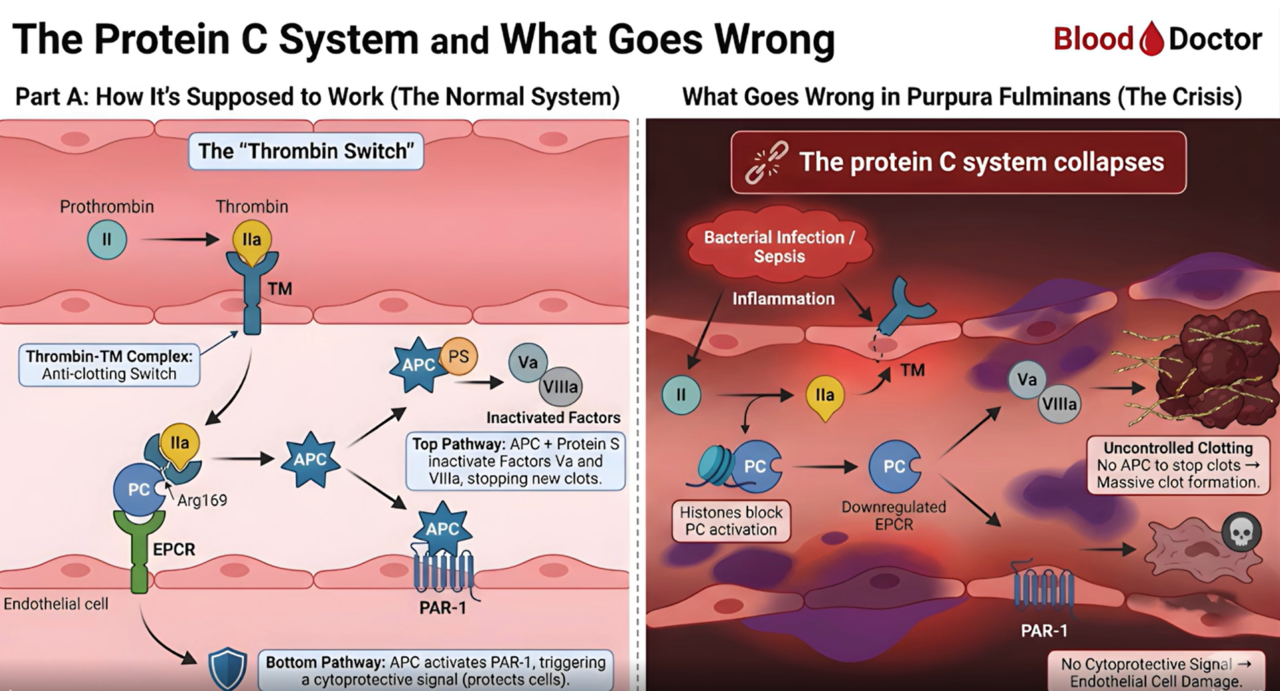
Normally, the endothelium is a pro-survival, antithrombotic surface. The “Thrombin Switch” is the central mechanism:
The Mechanism: Thrombin (IIa) binds to Thrombomodulin (TM) on the endothelial surface.
The Switch: This complex shifts thrombin’s substrate specificity away from fibrinogen and toward Protein C (PC).
The Result: PC is converted to Activated Protein C (APC). Along with its cofactor Protein S, it proteolytically inactivates Factors Va and VIIIa, halting the coagulation cascade.
Cytoprotection: APC also signals through PAR-1 and EPCR to activate anti-inflammatory and anti-apoptotic pathways.
Part 2: The Molecular Collapse (Pathophysiology of PF)
In severe sepsis—often triggered by Neisseria meningitidis—this elegant system suffers a total Pathophysiological Failure:
Receptor Shedding: Massive cytokine release triggers the proteolytic shedding of TM and EPCR from the endothelial surface. Without these anchors, PC cannot be activated.
Nuclear Interference: Neutrophil Extracellular Traps (NETs) release histones that directly inhibit the activation of the PC zymogen.
Consumption Coagulopathy: Unchecked thrombin generation consumes existing Protein C faster than hepatic synthesis can replenish it.
The Clinical Consequence: Maladaptive thromboinflammation. The resulting microvascular thrombosis leads to the characteristic purpuric skin necrosis and multi-organ failure.
Part 3: The Clinical Rescue (The “Blood Doctor” Protocol)
Management of this Molecular Collapse requires immediate, evidence-based intervention:
The Diagnostic Threshold: A PC activity level <40% in the context of rapidly progressing purpura is a critical diagnostic marker.
Precision Replacement: Administer Protein C Concentrate (100 units/kg). Our goal is a therapeutic target of >80% activity to restore the antithrombotic rheology.
The Anticoagulation Paradox: While the patient may appear to have a bleeding diathesis, we must address the underlying “thrombin storm” with Heparin (monitored via anti-Xa) to salvage the microcirculation.
Summary for the Haematology Community
Purpura Fulminans represents the ultimate “tipping point” where the cross-talk between coagulation and innate immunity becomes lethal. Recognizing the Systemic Dysregulation of Protein C early is the difference between limb salvage and mortality.
To my fellow Haematologists: In your practice, do you prioritize PC concentrate or FFP as the primary replacement bridge in the first 6 hours?”
Find more posts featuring Abdul Mannan on Hemostasis Today.
-
Feb 23, 2026, 11:37Charles Okyere Boadu: Blood Donation Helps Lower Your Risk of Stroke and Organ Damage
-
Feb 23, 2026, 11:29Emma Lefrancais: Uncovering A Key Role for The IL-33/ST2 Axis in Platelet Biology with Lucie Gelon
-
Feb 22, 2026, 14:16Ilenia Calcaterra: From Representation to Intellectual Independence in Women in Science
-
Feb 22, 2026, 13:27Pete Stibbs: New AHA and ACC PE Guidelines Finally Align with Real Clinical Practice
-
Feb 22, 2026, 10:39Tagreed Alkaltham: Fibrinogen Concentrate Is a Deliberate Clinical Choice in Acute Bleeding
-
Feb 22, 2026, 09:38Abdulrahman Nasiri: Significant Shifts In The 2026 AHA/ACC Guidelines for Acute Pulmonary Embolism
-
Feb 22, 2026, 09:22Shiny K. Kajal: Not All Transfusion Reactions Are Immunohematologic Incompatibilities
-
Feb 22, 2026, 09:12Arun V J։ The Hidden Risks in Every Blood Bag
-
Feb 22, 2026, 08:56Parandzem Khachatryan։ How Hard Is It to Be a Mom, a Wife, a Professor, and a Doctor All at Once?

