Time and Severe Hypoperfusion: 2 Threats for Hemorrhagic Transformation in Stroke
International Journal of Stroke (IJS) recently shared a post on X:
”Just Accepted!
Study finds hemorrhagic transformation was associated with onset-to-imaging time and presence of severe hypoperfusion. No interaction found between time and severe hypoperfusion.”
Read the full article here.
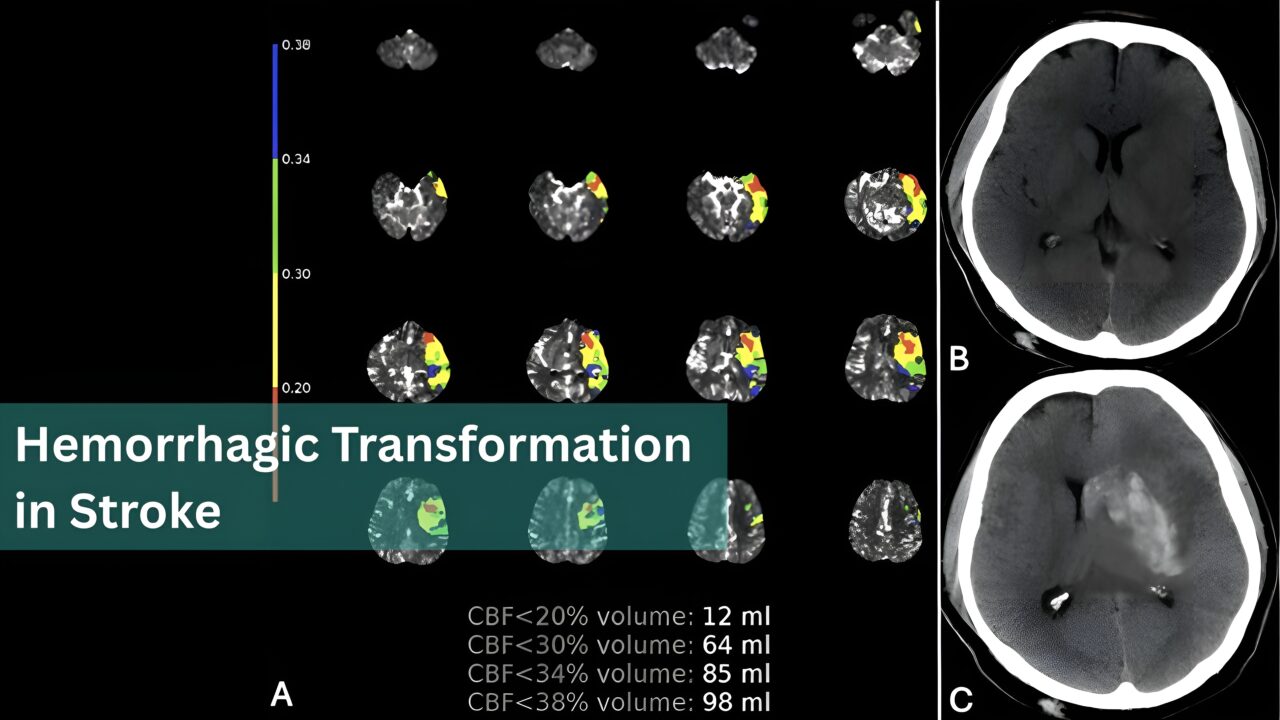
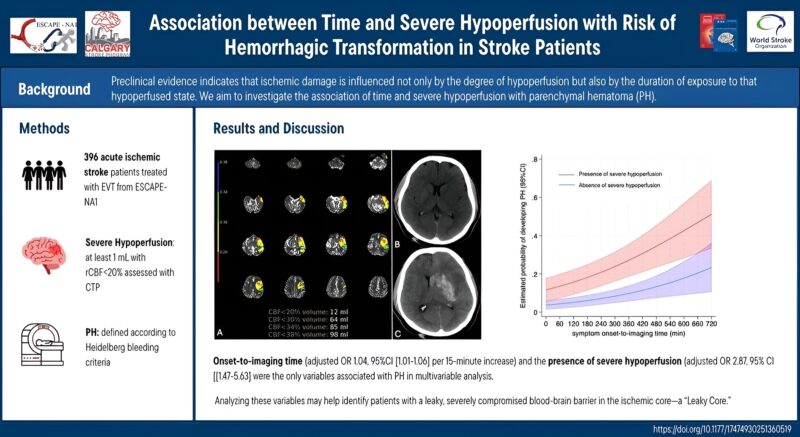
A new study is reinforcing the importance of timely management of stroke in an article ‘Association between Time and Severe Hypoperfusion with Risk of Hemorrhagic Transformation in Stroke Patients’ by Umberto Pensato et al., published in International Journal of Stroke (IJS).
Emerging evidence highlights that both severe hypoperfusion and time spent in a hypoperfused state contribute to the risk of parenchymal hematoma (PH) in ischemic stroke.
A recent analysis confirms that while each factor independently increases the likelihood of hemorrhagic transformation (HT), their interaction was not statistically significant.
These findings suggest that the risk of HT is influenced by distinct pathways related to hypoperfusion severity and duration.
Identifying patients with a “leaky core”—those with severely compromised blood-brain barriers—could enhance patient selection for targeted interventions!
Hemostasis Today, your daily update on scientific advancements in the World of Stroke.
-
Feb 5, 2026, 17:35Shiny K. Kajal: ELISA vs CLIA vs NAT – Comparison of Screening Test for TTis
-
Feb 5, 2026, 17:31Bartosz Hudzik: Top 10 Advances in Thrombosis and Antithrombotic Therapy in 2025
-
Feb 5, 2026, 17:27Jecko Thachil: A Historical Perspective on Iron Deficiency Anaemia in Women
-
Feb 5, 2026, 17:14WFH Annual Global Survey Identifies Over 112,000 Women and Girls With Bleeding Disorders
-
Feb 5, 2026, 16:22Muthukumar R: What if One Blood Test Could Tell Doctors Much More Than it Does Today?
-
Feb 5, 2026, 16:20Emmanuel J Favaloro: New Study on Biomarkers for Coagulation Disorders
-
Feb 5, 2026, 16:18Maxime Dely: Trends in Red Blood Cell Consumption in France
-
Feb 5, 2026, 16:17Shervin Jose: How Herbal Medicine Changed World History
-
Feb 5, 2026, 16:12Ahmed Koriesh: Stroke Primary Prevention – Questions We Hear Every Day

