
Dr. S.0 MIKAYE/LinkedIn
Dec 10, 2025, 14:08
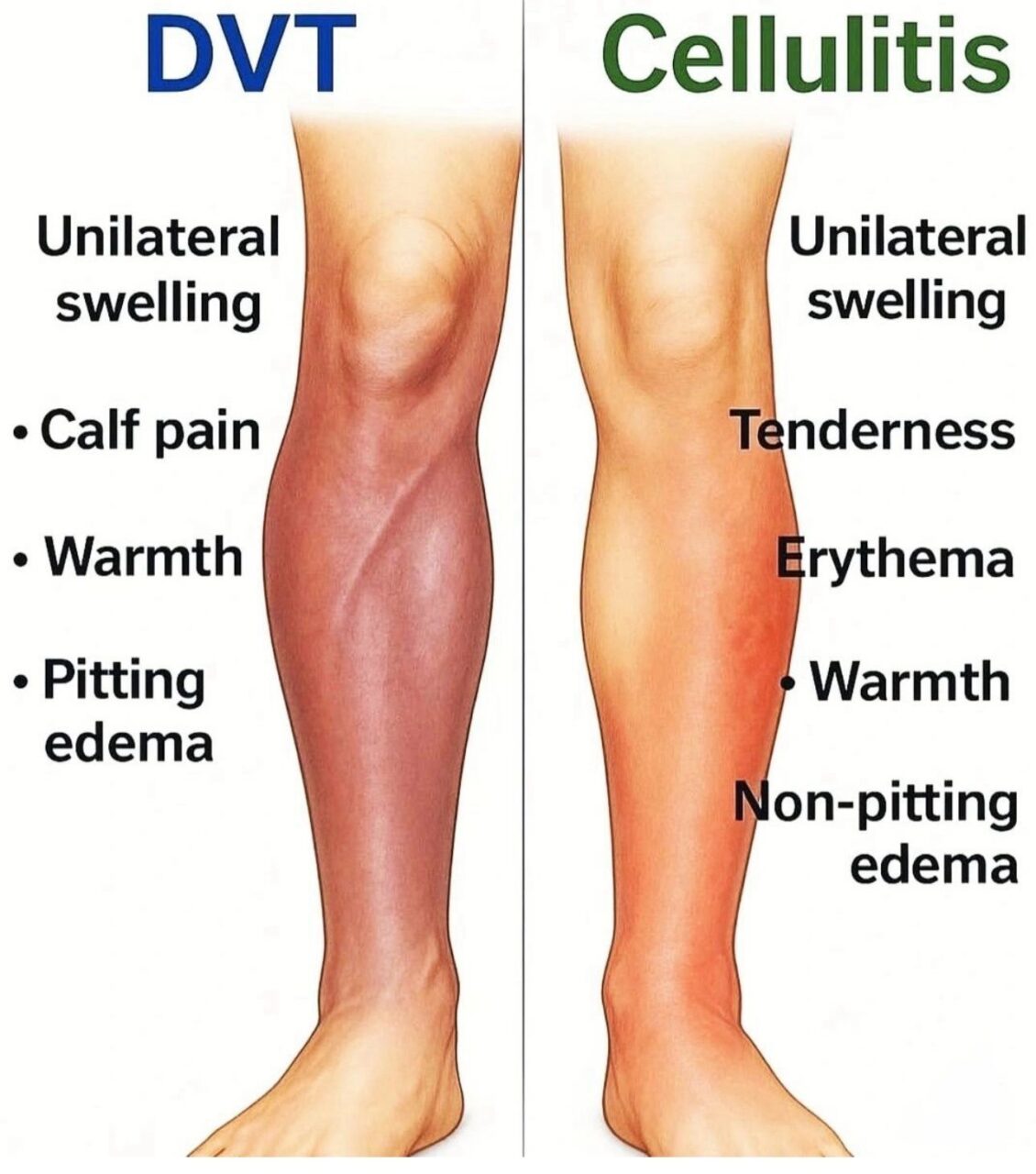
Samwel Mikaye: Overview of Deep Vein Thrombosis (DVT) and Cellulitis
Samwel Mikaye, CEO of SaMik Medical Center, posted on LinkedIn:
“Overview of Deep Vein Thrombosis (DVT) and Cellulitis
1. Deep Vein Thrombosis (DVT)
Definition
- Formation of a blood clot in a deep vein, usually in the lower extremities (calf, thigh).
Risk Factors (Virchow’s Triad)
- Venous stasis: Immobility, long flights, hospitalization
- Endothelial injury: Trauma, surgery, central lines
- Hypercoagulable state: Pregnancy/postpartum, cancer, inherited thrombophilia, oral contraceptives
Clinical Features
- Unilateral leg swelling (most common)
- Pain or tenderness, often calf pain
- Warmth and erythema over affected area
- Positive Homan’s sign (pain on dorsiflexion) – not reliable
Diagnosis
- D-dimer: Useful to rule out in low-risk patients
- Compression ultrasonography: Gold standard
- Venography: Rarely used, invasive
Management
- Anticoagulation (first-line):
• LMWH (enoxaparin) or fondaparinux initially
• Transition to warfarin (target INR 2–3) or DOACs (rivaroxaban, apixaban) - Supportive care:
• Leg elevation
• Compression stockings - Severe cases / complications:
• Thrombolysis for massive DVT
• IVC filter if anticoagulation contraindicated
2. Cellulitis
Definition
- Acute, spreading infection of the dermis and subcutaneous tissue, usually caused by Streptococcus pyogenes or Staphylococcus aureus.
Risk Factors
- Skin breaks: cuts, ulcers, insect bites
- Chronic edema, venous insufficiency, lymphedema
- Immunocompromised states: diabetes, HIV, chemotherapy
Clinical Features
- Red, warm, swollen, tender area
- Often unilateral, poorly demarcated
- May have fever, malaise, lymphangitis
- Rarely: bullae, necrosis (if severe or necrotizing infection)
Diagnosis
- Clinical diagnosis (no routine imaging required)
- Blood cultures if severe or systemic infection
- Consider ultrasound to rule out abscess
Management
- Antibiotics (empirical, based on severity):
• Mild: Oral cephalexin or dicloxacillin
• Severe: IV cefazolin, oxacillin, or vancomycin (if MRSA suspected) - Supportive care:
• Elevate affected limb
• Analgesia - Monitor for complications:
• Abscess formation → incision and drainage
• Necrotizing infection → surgical emergency”
Get the latest with Hemostasis Today.
-
Jan 31, 2026, 16:35IV Thrombolysis Does Not Improve Vision in Acute CRAO: Ahmed Koriesh on TenCRAOS Study
-
Jan 31, 2026, 16:24Joyce John Chalakkal: The Dangerous Area of The Face….
-
Jan 31, 2026, 16:04Rayya Saadiq Reflects On Qatar Health Congress 2026
-
Jan 31, 2026, 15:12Amar Raval on Oral Thin Film Drug Delivery Systems for Thrombosis Therapy
-
Jan 31, 2026, 14:40Heghine Khachatryan on WFH’s Call to Advance Health Equity for People with Bleeding Disorders
-
Jan 31, 2026, 14:10Emilia Arturo: Snake Venom, Clotting, and CryoEM!
-
Jan 31, 2026, 08:13Ming Y Lim On The Value of National Mentorship
-
Jan 31, 2026, 06:37Christian Schulze Presents The Post-Hoc Analysis of the DanGer Shock Trial
-
Jan 31, 2026, 06:27Negative Trials Matter: Anne Hege Aamodt Shares The TenCRAOS Trial

