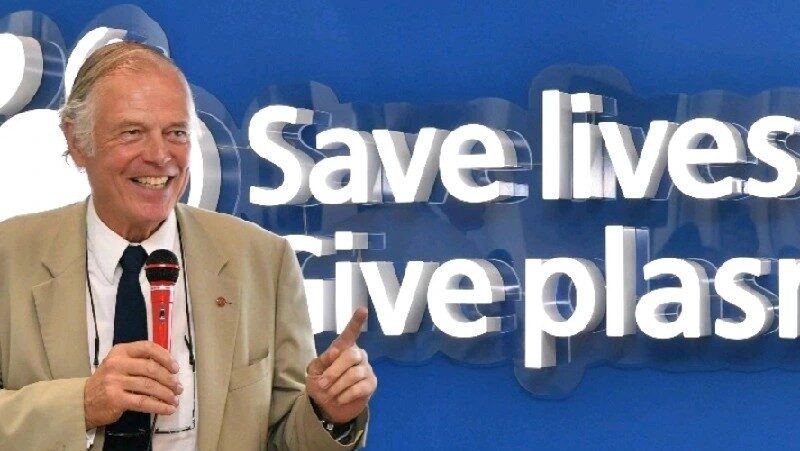
David McIntosh Highlights Global Blood Shortages and Fresh vs Stored RBCs
David McIntosh, Founder and Chair at United Plasma Action, reposted from Archil Jaliashvili on LinkedIn:
“This is most interesting work.
However, I repost it with a warning.
What the World is desperately short of right now is a satisfactory supply of red cells – for uses where nothing else will do.
Fresh blood is better than older stored blood – especially for neonates.
We all know that. What’s really fatal is no blood at all.
In about 90% of all cases globally there IS NOT ENOUGH BLOOD.
Therefore, where choices have to be made; where priorities have to be set; the top priority has to be MORE BLOOD PLEASE.
Let’s not get distracted from that fact by anything … not by anything at all, until every blood bank in every hospital in the World has ample stocks.”
Archil Jaliashvili shared in Pharmaceutical & Medical Network: Biotech, Healthcare, Pharma, Devices, Science, Jobs, Events and News public group on LinkedIn:
“What does a blood transfusion actually remedy?
In extreme hemodilution and hemorrhagic shock, focusing on the difference between fresh and stored RBCs.
Core Findings:
Clinically, transfusions are aimed at restoring oxygen-carrying capacity.
– Fresh RBC’ s restore both microvascular perfusion and oxygen capacity;
– Stored RBCs often restore viscosity but less effectively support microvascular perfusion and oxygenation.
Oxygen Affinity (p50)
– Stored RBCs lose 2,3-DPG.
RBC Storage Lesion
Progressive loss of deformability, ATP depletion, morphological changes, microvesicle shedding, increased aggregation, higher free hemoglobin.
These changes reduce FCD, impair O₂ delivery despite normal systemic parameters, and may cause vasoconstriction via NO scavenging.
NO Bioavailability
Hemolysis and free Hb from stored RBCs bind NO → vasoconstriction, reduced perfusion, and potential cardiovascular risk.
NO levels can recover in vivo, but the transient deficiency may be clinically important.
Experimental Conclusions
Fresh RBCs are consistently superior to stored RBCs in animal models — particularly for restoring microvascular perfusion and oxygenation.
The survival benefit may depend as much on restoring FCD as on oxygen capacity.
Clinical transfusion triggers based solely on hemoglobin may overlook perfusion deficits.
Why it matters – Oxygen Bridge: A Bridge to Recovery
BHOC – Biological Hemoglobin Oxygen Carrier.
-No Cross-Matching Required – Ready for immediate use in emergencies.
-High Oxygen-Carrying Efficiency and good perfusion.
-Immediate Restoration of Oxygenation – No need for factors like 2,3-DPG to function.
-Universal Complement to any cases where need efficient oxygenation.
Why it’s key: BHOC is not just a transfusion substitute — it’s an oxygen bridge, ensuring life-saving oxygen delivery in critical moments, from trauma to surgery, when every second counts.
Link to company.

Stay informed with Hemostasis Today.
-
Feb 28, 2026, 17:03Investing in Education, Prevention, and Lifesaving Research for a Healthier Tomorrow – AHA
-
Feb 28, 2026, 17:00Pamela Gavin: 1 in 10 Americans Live With A Rare Disease – That Is Not Rare, That Is Public Health
-
Feb 28, 2026, 16:59Thomas Rocco Jr: Exploring Agentic AI in Cardiovascular Medicine
-
Feb 28, 2026, 16:50Rob Maloney: Normalcy Is Not A Small Thing In Rare Disease
-
Feb 28, 2026, 16:49Céline Chapelle: Evaluating 6-Month Risks of Recurrent VTE and Major Bleeding With Tinzaparin
-
Feb 28, 2026, 16:46Nicolas Hulscher: Nattokinase Dissolves 84% of Amyloid Microclots In Vitro
-
Feb 28, 2026, 16:46Alfonso Tafur: Preventing Post-Hospitalization Blood Clots Using Precision Tools and Systems
-
Feb 28, 2026, 16:39Anel Karisik: Do Antidepressants Influence Swallowing Recovery After Acute Ischemic Stroke?
-
Feb 28, 2026, 16:38Akinchan Bhardwaj: Targeting SBK2 for Selective Inflammasome Resolution in Atherosclerosis

