AI generated
Feb 16, 2026, 13:56
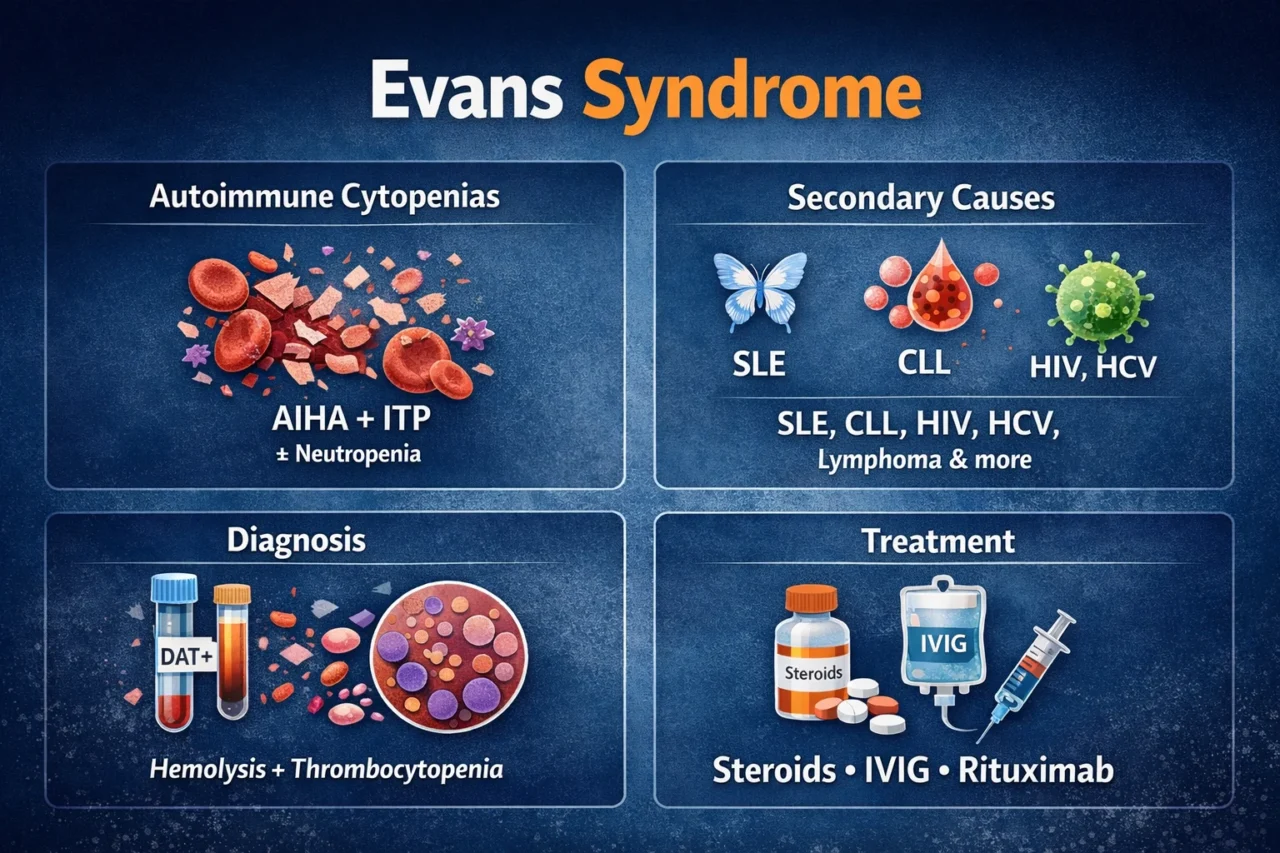
Chokri Ben Lamine: Evans Syndrome Key Clinical Insights
Chokri Ben Lamine, Adult Hematology and SCT Assistant Consultant at Oncology Center of Excellence at King Faisal Specialist Hospital and Research Center, shared a post on X.
“Evans Syndrome – High-Yield Tweet Pearls (Autoimmune hemolytic anemia with immune thrombocytopenia, with or without neutropenia)
- Definition: Presence of at least two autoimmune cytopenias
- Classic: AIHA and ITP
- With or Without Autoimmune neutropenia
- Can be simultaneous or sequential
- Chronic and relapsing course common
Pathophysiology
- Loss of immune tolerance
- Autoantibodies against RBCs and platelets
- Often polyclonal B-cell activation
- T-reg dysfunction implicated
- Secondary forms frequent
Secondary Causes (ALWAYS Screen)
- SLE
- CLL
- CVID
- ALPS
- Lymphoma
- Chronic infections (HIV, HCV)
- CTD spectrum
- Post-transplant immune dysregulation
Diagnosis
- DAT positive (warm AIHA commonest)
- Elevated LDH
- Increased Indirect bilirubin
- Reduced Haptoglobin
- Reticulocytosis (unless marrow suppressed)
- Isolated thrombocytopenia component
- Bone marrow usually compensatory
Differential
- TTP (schistocytes!)
- DIC
- Drug-induced cytopenia
- Aplastic anemia
- Hypersplenism
Treatment
- First-line: Steroids
- Prednisone 1–2 mg/kg
- IVIG for severe thrombocytopenia
- Transfuse RBCs if symptomatic
- Platelets if life-threatening bleed
Second-Line
- Rituximab (strong evidence)
- Splenectomy (selected)
- MMF
- Azathioprine
- Cyclosporine
- Sirolimus (emerging data)
- Thrombopoietin agonists in refractory ITP component
Severe Disease
- Can progress to multi-lineage cytopenia
- Infection risk high (from therapy and disease)
- Monitor IgG levels
- Vaccinate if planning splenectomy
Prognosis
- Chronic relapsing pattern typical
- Secondary forms have worse outcome
- Mortality mainly from infection or bleeding
- Early recognition and secondary workup critical
MCQ
Key diagnostic clue in Evans syndrome?
- Schistocytes
- DAT positive and thrombocytopenia
- Severe coagulopathy
- Pancytopenia with hypocellular marrow
Answer: B
OSCE Scenario
35-year-old with fatigue and petechiae
Hb 7 g/dL, Platelets 18 ×10⁹/L
DAT positive
- Start steroids immediately
- Screen for SLE/CLL/HIV
- Consider IVIG if bleeding
- Plan rituximab if steroid-refractory
Bottom Line
- Evans: autoimmune multi-lineage cytopenia
- Treat aggressively
- Always search for secondary cause”
Find more posts featuring Chokri Ben Lamine on Hemostasis Today.
-
Feb 16, 2026, 13:51Adela Castro: 2025 EULAR Guidelines Key Updates in Lupus Nephritis
-
Feb 16, 2026, 13:50Rosa Hart: Stop Waiting For A Seat And Start Shaping The Table
-
Feb 16, 2026, 13:49Harprit Singh: India’s Silent Transfusion Gap – What Policymakers Need to Know in 2026
-
Feb 16, 2026, 13:46A Conversation on Gene Therapy in Hemophilia B – Irish Haemophilia Society
-
Feb 16, 2026, 13:45Nathan Connell Speaks on Gender Diversity In Haemostasis Care at EAHAD 2026
-
Feb 16, 2026, 13:40David McIntosh: Concrete Performance Targets for Rare Disease Patients
-
Feb 16, 2026, 13:40Ramy Abdelnaby: Exploring The Timing of Antiplatelet Administration In Minor Stroke Post-Thrombolysis
-
Feb 16, 2026, 13:33Anne Hege Aamodt Congratulates Gisle Berg Helland on PhD Defense About Stroke Outcome MRI and ML Prediction
-
Feb 16, 2026, 13:25Rucha Patil: Delighted to Contribute to The Round Table on Integrated Care of Hemophilia and Hemoglobinopathies

