
Mohamed Magdy Badr: When Blood Disorders Break the Skin
Mohamed Magdy Badr, Wound Care Consultant at Armed Force Rehabilitation Center, posted on LinkedIn:
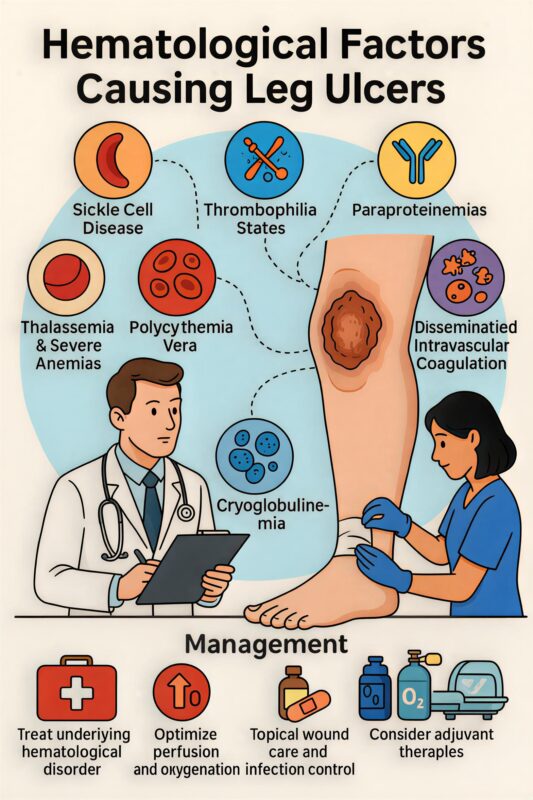
”When Blood Disorders Break the Skin – Hematologic Causes of Leg Ulcers
1. Sickle Cell Disease (SCD)
Mechanism: Vaso-occlusion and chronic hemolytic anemia → tissue ischemia and poor oxygen delivery.
Features:
- Common around the medial or lateral malleolus.
- Painful, punched-out ulcers with hyperpigmented margins.
- Delayed healing, often recurrent.
Other clues: Anemia, reticulocytosis, leg swelling, history of painful crises.
2. Thalassemia and Severe Anemias
Mechanism: Chronic hypoxia and iron overload → impaired collagen synthesis and tissue repair.
Ulcer characteristics:
- Usually shallow with pale granulation tissue.
- Often associated with hemosiderosis and fragile skin.
3. Polycythemia Vera
Mechanism: Hyperviscosity and microthrombi → tissue ischemia.
Typical lesions:
- Painful, necrotic ulcers (often on lower legs).
- May worsen with hydroxyurea therapy (drug-induced ulcers).
4. Leukemia and Myeloproliferative Disorders
Mechanism: Leukostasis, anemia, thrombocytopenia → poor perfusion + impaired immunity.
Findings:
- Necrotic ulcers, gangrenous changes.
- May present with leukemia cutis or neutrophilic dermatoses (Sweet’s syndrome, pyoderma gangrenosum-like lesions).
5. Thrombophilic States (Inherited or Acquired)
Examples:
- Antiphospholipid syndrome (APS)
- Factor V Leiden mutation
- Protein C/S deficiency
- Antithrombin III deficiency
Mechanism: Recurrent microvascular thrombosis → ischemic ulceration.
- Clinical features: Livedo reticularis, painful ulcers, history of miscarriages or DVTs (especially in APS).
6. Cryoglobulinemia and Cold Agglutinin Disease
Mechanism: Immune complex deposition → small-vessel vasculitis → ulceration.
Features:
- Painful purpura, ulcers on acral parts (toes, heels).
- Triggered by cold exposure.
7. Paraproteinemias (e.g., Multiple Myeloma, Waldenström)
Mechanism: Hyperviscosity and immune complex deposition → vascular occlusion.
Findings: Livedo, ulcers, necrosis, poor wound healing.
8. Disseminated Intravascular Coagulation (DIC) / Thrombotic Microangiopathies
Mechanism: Microthrombosis → tissue ischemia and necrosis.
Seen in: Sepsis, malignancy, HELLP syndrome, TTP/HUS.
Lesions: Painful purpura → necrotic ulcers or gangrene.
Key Diagnostic Workup
- CBC, peripheral smear
- Reticulocyte count
- Coagulation profile
- ESR, CRP
- Autoimmune and thrombophilia screening (ANA, APL antibodies, Protein C/S, AT III)
- Serum electrophoresis for paraproteins
- Skin biopsy (if vasculitis or malignancy suspected)
Management Principles
- Treat the underlying hematologic disorder (transfusion, cytoreduction, anticoagulation, immunotherapy).
- Optimize perfusion and oxygenation.
- Meticulous local wound care and infection control.
- Compression therapy where safe.
- Adjuvant measures such as hyperbaric oxygen or pentoxifylline for resistant cases
Clinical Insight
When a “vascular” ulcer fails to heal despite proper blood flow, think hematologic.
“Healing the wound begins with healing the blood.” ”
Keep up with Hemostasis Today.
-
Feb 26, 2026, 15:58Daniel Victor Ortigoza։ Lipoprotein(a) Levels Predict Long-Term Cardiovascular Risk in Women
-
Feb 26, 2026, 15:51Augustina Isioma Ikusemoro: The Real Miracle in Trauma Care Happens Behind the Scenes
-
Feb 26, 2026, 15:42Jim Hoffman։ Targeting NETosis to Improve Perfusion and Reduce Thrombosis in AMI
-
Feb 26, 2026, 15:40Elvira Grandone: ISTH Launches An International Survey to Capture Real-World Practice of Pregnancy Anemia
-
Feb 26, 2026, 15:39Ashok Yadav: Placental Glycogen as a Vital Energy Reserve for Fetal and Placental Health
-
Feb 26, 2026, 15:37Nayab Ahmed: Main Reasons for Washing Platelet-Rich Plasma
-
Feb 26, 2026, 15:36Robert Negrin Shares His Outlook for the Year Ahead as ASH President
-
Feb 26, 2026, 15:24Nancy Shapiro: Excited to See This Publication on Current Landscape of Anticoagulation Stewardship Released
-
Feb 26, 2026, 15:15Ahmed Nasreldein: Stay Current on Key Updates in Ischemic and Hemorrhagic Stroke

