
PNH in Focus: Neepaja Canjiradan Discusses Hemolysis, Diagnostic Clues, and Complement Inhibitor Therapy
Neepaja Canjiradan, a clinical pathologist at AVM Labs, posted on LinkedIn:
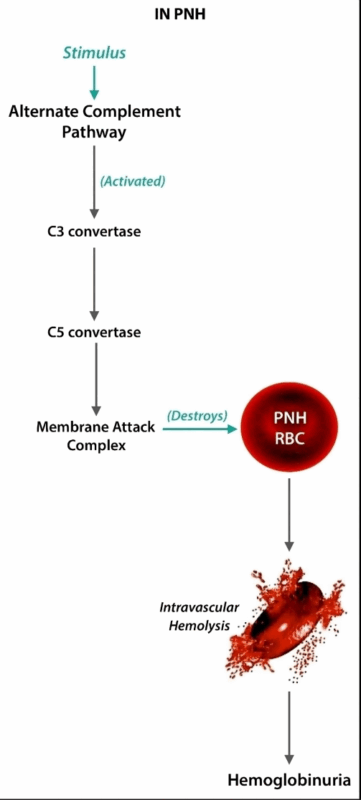
”Haematology series 17
Paroxysmal nocturnal Haemoglobinuria: The only condition where your urine says “Good Morning” darker than your coffee
On the Peripheral Smear
Hemolysis galore → bite cells, ghost cells, and the occasional schistocyte cameo.
Reticulocytosis – marrow working overtime like a resident on night duty.
Basically looks like “aftermath of a complement bar fight.”
In the Bone Marrow
Hypoplastic/aplastic in some, hyperplastic in others.
Erythroid hyperplasia = marrow screaming “I got this!” while clearly not.
Frequently hand-in-hand with aplastic anemia or MDS-PNH is never lonely.
Flow Cytometry (the Real MVP)
The mic-drop moment → loss of CD55 and CD59 on RBCs and granulocytes.
Forget the Ham test—flow cytometry is the Sherlock Holmes here.
Seeing that PNH clone pop up is equal parts diagnostic thrill and clinical reality check.
Treatment in a Nutshell
Big strides from IV infusions to oral therapies.
Complement inhibitors galore, but let the hematologists juggle the alphabet soup.
HSCT = still the only curative pathway.
Pathologist’s Humor Corner
PNH patients: “Why is my urine so dark in the morning?”
Pathologist: “Because your RBCs had a rough night.”
RBCs without CD55/CD59 → the ultimate example of what happens when you skip PPE.
Flow cytometry in PNH = Facebook relationship status: “It’s complicated.”
Bottom Line
Smear gives the clues,
Marrow shows the struggle,
Flow cytometry seals the deal.
PNH may be rare, but it keeps pathology exciting – diagnostics with just the right mix of science and sass.”
Stay updated with Hemostasis Today.
-
Feb 3, 2026, 10:53Aurelio Maggio: The Final Chapter of Our Journey Through Thalassemia
-
Feb 3, 2026, 10:40Pedro Perez: Post-Thrombectomy DVT Recovery in 2026 – Closing the Loop on Outcomes
-
Feb 3, 2026, 10:26Ryan Williams: This Article Brings to Light The Complexity of PRP…
-
Feb 3, 2026, 10:05Tiago Lopes: Can AI Predict Immune Reactions of New Drugs? Yes!
-
Feb 3, 2026, 09:51Rucha Patil Reflects on 49th MHG Annual Conference and Essence of ASH 2025
-
Feb 3, 2026, 09:37Grigoris Gerotziafas on VTE in MM and BCMA: We Are Pleased to Announce Our New Systematic Review
-
Feb 3, 2026, 09:24Early-Bird Registration for the WFH 2026 World Congress is Now Open
-
Feb 3, 2026, 09:15Joshua Bernstock: Prehospital Stroke Triage Has Hit a Ceiling
-
Feb 3, 2026, 09:00A Major Highlight of 2025 and Honour For Me: Ashkan Shoamanesh at Huashan International Stroke Conference

