
Tareq Abadl: Low Haptoglobin – Practical Lab Interpretation
Tareq Abadl, Medical Laboratory Specialist and Director of the Blood Bank at Dr. Abdelkader Al-Mutawakkil Hospital, shared a post on LinkedIn:
“Low Haptoglobin – Practical Lab Interpretation
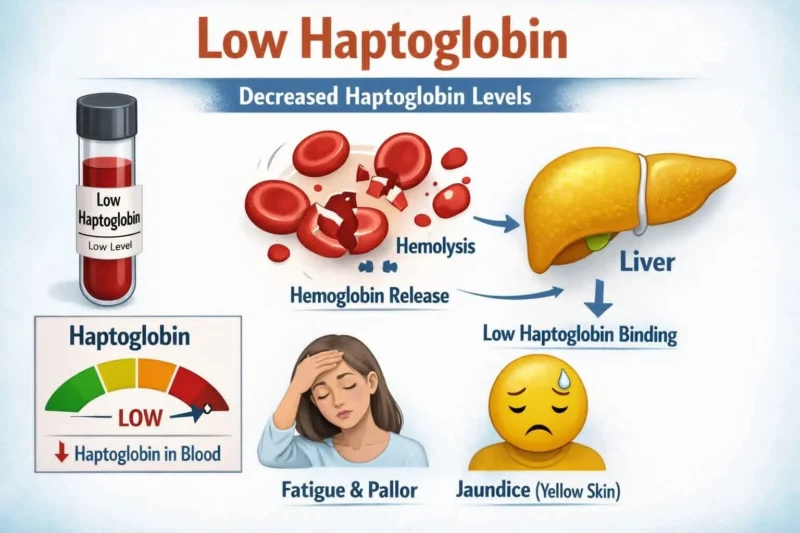
Haptoglobin binds free hemoglobin released into plasma during intravascular hemolysis.
A low level suggests hemolysis, but it is not specific and must be interpreted with the full lab pattern and clinical context.
1) Intravascular hemolysis
Ongoing or massive RBC destruction rapidly consumes haptoglobin.
Supportive lab pattern:
- Increased LDH
- Increased Indirect (unconjugated) bilirubin
- Decreased Haptoglobin
- Increased Reticulocyte count
Schistocytes / hemolytic features on blood smear
Lab pearl: If labs suggest hemolysis but the clinical picture (or ECG, vitals) doesn’t fit → pause and reassess before triggering urgent calls.
2) Liver disease
Haptoglobin is synthesized in the liver.
Advanced liver dysfunction → Decreased production → low haptoglobin without hemolysis
Always correlate with AST, ALT, ALP, bilirubin, INR
Key pitfall: Low haptoglobin ≠ hemolysis if the liver can’t make it.
3) Post-transfusion or delayed transfusion reaction
Hemolytic transfusion reactions can cause true intravascular hemolysis.
Always review:
- Recent transfusion history
- Timing of symptoms vs lab changes
Add-on tests if suspected:
- DAT (Direct Coombs)
- Plasma free hemoglobin
- Urine hemoglobin
4) Mechanical / device-related hemolysis
Seen with:
- ECMO
- Prosthetic heart valves
- Extracorporeal circuits
Shear stress → chronic intravascular hemolysis → persistently low haptoglobin
Trend matters more than a single value.
5) Pre-analytical & interpretation pitfalls
In vitro hemolysis (traumatic draw, delayed centrifugation, pneumatic tube transport) can falsely mimic hemolysis
Haptoglobin is an acute-phase reactant
→ Can be normal or high despite active hemolysis in inflammation or infection
Always check:
- Hemolysis index
- Sample quality
- Repeat on a clean specimen if uncertain
Quick Lab Workflow (Before Calling Clinicians )
- Check hemolysis index & sample integrity
- Review: CBC + smear, reticulocytes, LDH, total & indirect bilirubin, haptoglobin
- Ask about transfusions, valves, ECMO, devices
- If unclear → recommend repeat testing + clinical correlation
When hemolysis stops, haptoglobin typically recovers over days to weeks — recheck per protocol.
Normal Reference Range (Important!)
Haptoglobin (adult):~30–200 mg/dL (≈ 0.3–2.0 g/L)
Ranges vary by laboratory and method — always use local reference values.
Extra High-Yield Pearls
Congenital anhaptoglobinemia → chronically undetectable haptoglobin (rare but real)
Extravascular hemolysis (e.g., hypersplenism) may have normal haptoglobin
Haptoglobin alone should never be used to diagnose hemolysis.”
More posts from Tareq Abadl on Hemostasis Today.
-
Feb 7, 2026, 15:58New Study Reveals Higher-Than-Expected Prevalence of Factor VII Deficiency – RPTH Journal
-
Feb 7, 2026, 15:29Rowan Paul: MSCs Show Strongest Pain Reduction in Regenerative Medicine Approaches
-
Feb 7, 2026, 15:24Abeer Alanazi: Asundexian Reduces Stroke and Mortality Without Increased Bleeding
-
Feb 7, 2026, 15:19Shabbir Ansari: Rare F3 Missense Variants Markedly Impair Coagulation Initiation
-
Feb 7, 2026, 15:13Caitlin Raymond: Understanding Risks in Rare Group A Subtypes with Anti-A1 Antibodies in Transfusion Medicine
-
Feb 7, 2026, 14:57Akinchan Bhardwaj։ OCEANIC-STROKE Trial Signals a New Era in Secondary Stroke Prevention
-
Feb 7, 2026, 14:32Ming Y Lim: Launching a Virtual Iron Deficiency Clinic at the University of Utah School of Medicine
-
Feb 7, 2026, 14:30Exploring Thrombin Generation Profiling in Rare Coagulation Factor Deficiencies – JTH
-
Feb 7, 2026, 14:25C Michael Gibson: Asundexian Reduces Ischemic Stroke Without Increasing Bleeding Risk

