
Abdul Mannan: When Gender Bias Becomes a Diagnostic Error – Inherited Bleeding Disorders are Still Being Missed
Dr Abdul Mannan, Consultant Haematologist at Betsi Cadwaladr University Health Board, shared a post on LinkedIn:
“When Gender Bias Becomes a Diagnostic Error
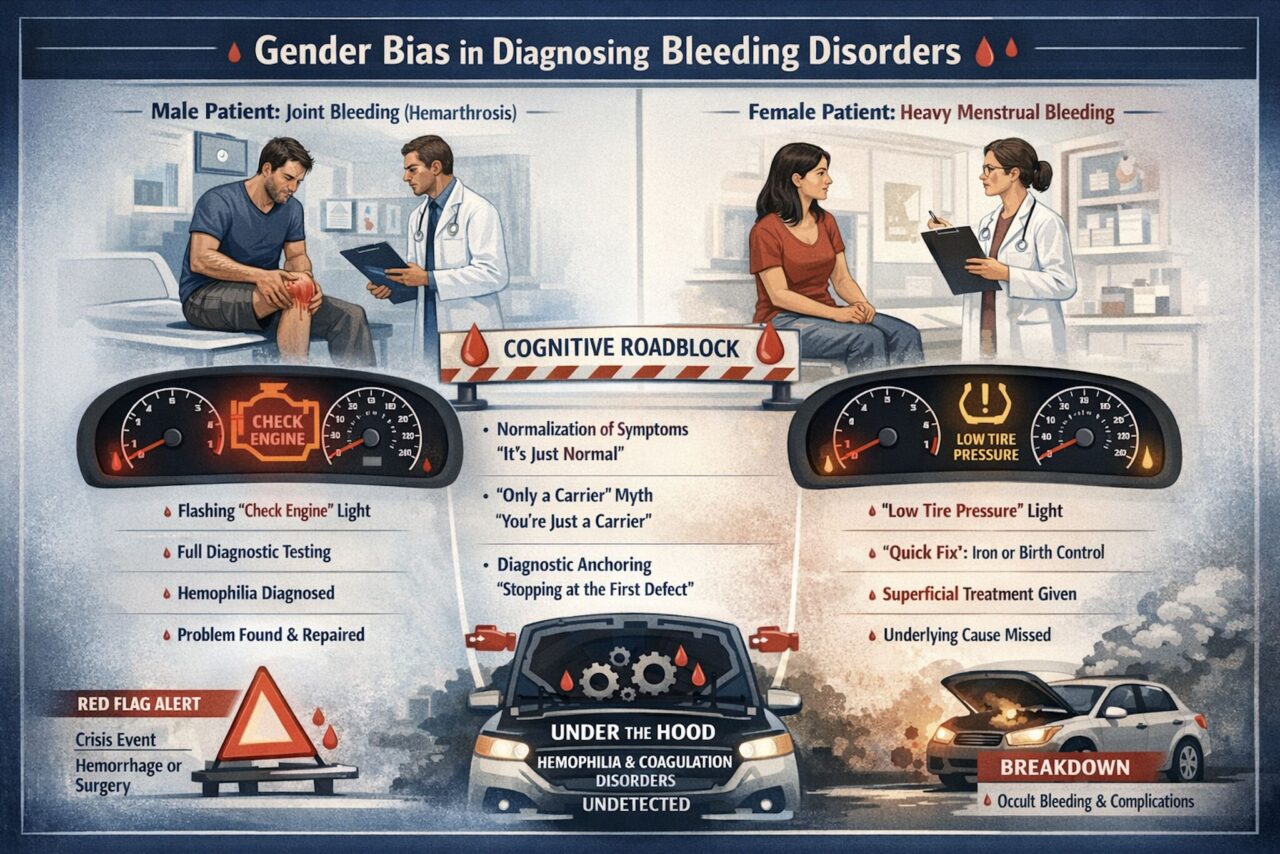
Inherited Bleeding Disorders are still being missed. Not because tests don’t exist. But because thinking stops too early.
In bleeding disorders, biology is not the only barrier.
Cognitive bias is.
Same system. Same disease risk. Very different responses.
When a man presents with joint bleeding, alarms go off.
Full coagulation work-up. Factor levels. Genetics. Diagnosis.
When a woman or girl presents with heavy menstrual bleeding, the response is often very different:
“It’s normal.”
“It runs in the family.”
“It’s gynaecological.”
“Try iron. Try hormones.”
And the hood never gets opened.
These are not knowledge gaps. They are cognitive roadblocks:
- Normalization of symptoms
Generational bleeding is mistaken for “family traits” rather than inherited disease. - The ‘only a carrier’ myth
Women with hemophilia genes are still assumed to be asymptomatic, despite clear evidence to the contrary. - Satisfied search error
Find mild vWD → stop investigating
Miss the second defect → label as “treatment-resistant”
- Physiological masking
Pregnancy normalizes factor levels → false reassurance → delayed postpartum hemorrhage. - Menstrual stigma
If bleeding isn’t quantified, it isn’t taken seriously.
A pad every 30 minutes becomes “just a heavy period”.
Think of it like this:
A man with hemarthrosis gets a flashing check engine light.
A woman with HMB gets a low tyre pressure warning.
One triggers diagnostics.
The other gets a quick fix.
Until the breakdown happens — surgery, childbirth, hemorrhage.
Key message:
Treatment failure in women is not “difficult anatomy”.
It is a red flag.
What changes outcomes?
- Structured bleeding assessment tools
- Factor levels in symptomatic “carriers”
- Looking for combined defects
- Testing outside pregnancy
- Taking menstrual bleeding seriously — clinically, not culturally
This infographic isn’t about blame.
It’s about where our thinking stops too soon.
If we don’t challenge these cognitive shortcuts, women with inherited bleeding disorders will continue to be diagnosed late, during crises, or not at all.
Blood Doctor
Because bleeding disorders don’t respect gender — but bias still does.”
Get more insights from Abdul Mannan with Hemostasis Today.
-
Feb 17, 2026, 16:34ISTH Names Five Global Recipients of 2026 Esteemed Career Awards
-
Feb 17, 2026, 16:16Flora Peyvandi: A Multicenter Initiative to Improve Guideline Adherence in Pediatric ITP
-
Feb 17, 2026, 16:14Hendrianus The: Intravenous Cangrelor in Hemodynamically Unstable Patients Undergoing PCI
-
Feb 17, 2026, 15:42Paul Wischmeyer: Nutrient Absorption in the GI Tract
-
Feb 17, 2026, 15:40Mahesan Subramaniam: Reversing Age-Related Decline in Blood Stem Cells
-
Feb 17, 2026, 15:38Wolfgang Miesbach: How a Single Mutation Can Flip Immunity into VITT
-
Feb 17, 2026, 15:34Jeff June: When Safety Warnings Outlive the Evidence – What Statins Teach Us About Stroke Prevention and Biology
-
Feb 17, 2026, 15:32Gabrielle Sarlon: Key Messages to Improve VTE Management in Women of Childbearing Age
-
Feb 17, 2026, 15:27Piezo1 Gain-of-Function Mutation Explains Thromboembolic Complications in Hereditary Xerocytosis – JTH

