
Mohamed Magdy Badr: How Do Acute Wounds Turn Into Chronic Wounds?
Mohamed Magdy Badr, Wound Care Consultant at Armed Force Rehabilitation Center, posted on LinkedIn:
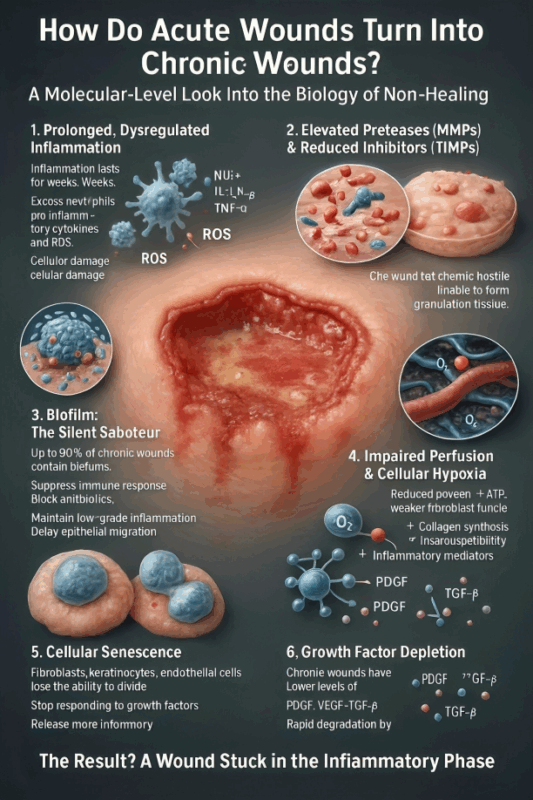
”How Do Acute Wounds Turn Into Chronic Wounds?
A Molecular-Level Look Into the Biology of Non-Healing
Not all wounds heal the same. Some progress smoothly through hemostasis, inflammation, proliferation, and remodeling. Others become stuck, turning into chronic, non-healing wounds that persist for months.
But the real story starts at the molecular level.
1. Prolonged, Dysregulated Inflammation
- In normal healing, inflammation lasts 48–72 hours.
- In chronic wounds, inflammatory cells remain activated for weeks.
- Excess neutrophils release destructive enzymes
- Continuous production of pro-inflammatory cytokines (IL-1, IL-6, TNF-α)
- Increased ROS → cellular damage
This creates a toxic, self-perpetuating loop.
2. Elevated Proteases (MMPs) and Reduced Inhibitors (TIMPs)
Chronic wounds show:
- High MMPs → degrade extracellular matrix, growth factors, and new tissue
- Low TIMPs → no balance
Result: the wound bed becomes chemically hostile, unable to form granulation tissue.
3. Biofilm: The Silent Saboteur
- Up to 80% of chronic wounds contain biofilms.
- Biofilm communities:
- Suppress immune response
- Block antibiotics
- Maintain low-grade inflammation
- Delay epithelial migration
This keeps the wound locked in an inflammatory state.
4. Impaired Perfusion and Cellular Hypoxia
Reduced oxygen affects every molecular step:
- ↓ ATP → weaker fibroblast function
- ↓ collagen synthesis
- ↑ susceptibility to infection
- ↑ inflammatory mediators
Hypoxia changes the entire gene expression profile of the wound.
5. Cellular Senescence
- Fibroblasts, keratinocytes, and endothelial cells become senescent:
- Lose ability to divide
- Stop responding to growth factors
- Release more inflammatory cytokines (SASP phenotype)
- The wound essentially loses its “healing machinery.”
6. Growth Factor Depletion
Chronic wounds have:
- Lower levels of PDGF, VEGF, TGF-β
- Poor receptor response
- Rapid degradation by proteases
Without these signals, angiogenesis, epithelialization, and matrix formation cannot progress.
The Result? A Wound Stuck in the Inflammatory Phase
Instead of moving to proliferation, the wound becomes trapped in a molecular cycle of:
- Persistent inflammation
- Biofilm activity
- Cellular senescence
- Enzymatic imbalance
- Poor perfusion
This is how an acute wound transforms into a chronic one.
Final Message
Understanding the molecular biology of chronic wounds isn’t academic — it is essential for designing better treatments, selecting smarter dressings, breaking biofilms, and improving patient outcomes.”
Stay informed with Hemostasis Today.
-
Feb 23, 2026, 18:13Fight4Hematology Supports Research and Empowers the Next Generation – ASH
-
Feb 23, 2026, 17:59Wolfgang Miesbach: Real-World Evidence of Emicizumab on Joint Outcomes in Hemophilia A
-
Feb 23, 2026, 17:56Shiny K Kajal: The Transfusion Reaction We Often Miss
-
Feb 23, 2026, 17:53Radheshyam Meher: Contributing to the Transfusion Evidence Round-Up for International Childhood Cancer Day 2026
-
Feb 23, 2026, 17:46Mahesan Subramaniam: The Physiological Impact of Anger on Immunity
-
Feb 23, 2026, 17:42Bryan Fry: First Evidence That Bothrops atrox Venom Directly Activates Human Factor VII
-
Feb 23, 2026, 17:34Bastu Odoka: Why Blood Should NOT be Left at the Bedside to ‘Warm’
-
Feb 23, 2026, 17:28Henry Burkitt: Patients Are Challenging How the Medicines Policy System Works in England
-
Feb 23, 2026, 16:50Mutaz Al‑Sabah: Interesting Webinar on FH in Women is Now Available to Watch

