
Rachel Rosovsky on New Research Linking Depression and Anxiety to Cardiovascular Risk
Rachel Rosovsky, Hematologist, Expert in Thrombosis (PE/DVT) and Hemostasis at Massachusetts General Hospital, shared a post by Shady Abohashem on LinkedIn, adding:
“Honored to be involved in this important research which not only highlights the link between depression and anxiety and risk of cardiovascular events, but also explores the underlying mechanisms.”
Quoting Shady Abohashem‘s post
“Depression and Anxiety don’t stop at the brain. They can get under your skin and affect the Heart.
For years, mental health and cardiovascular disease have been treated as separate domains. But growing evidence suggests they are deeply connected, biologically, not just behaviorally.
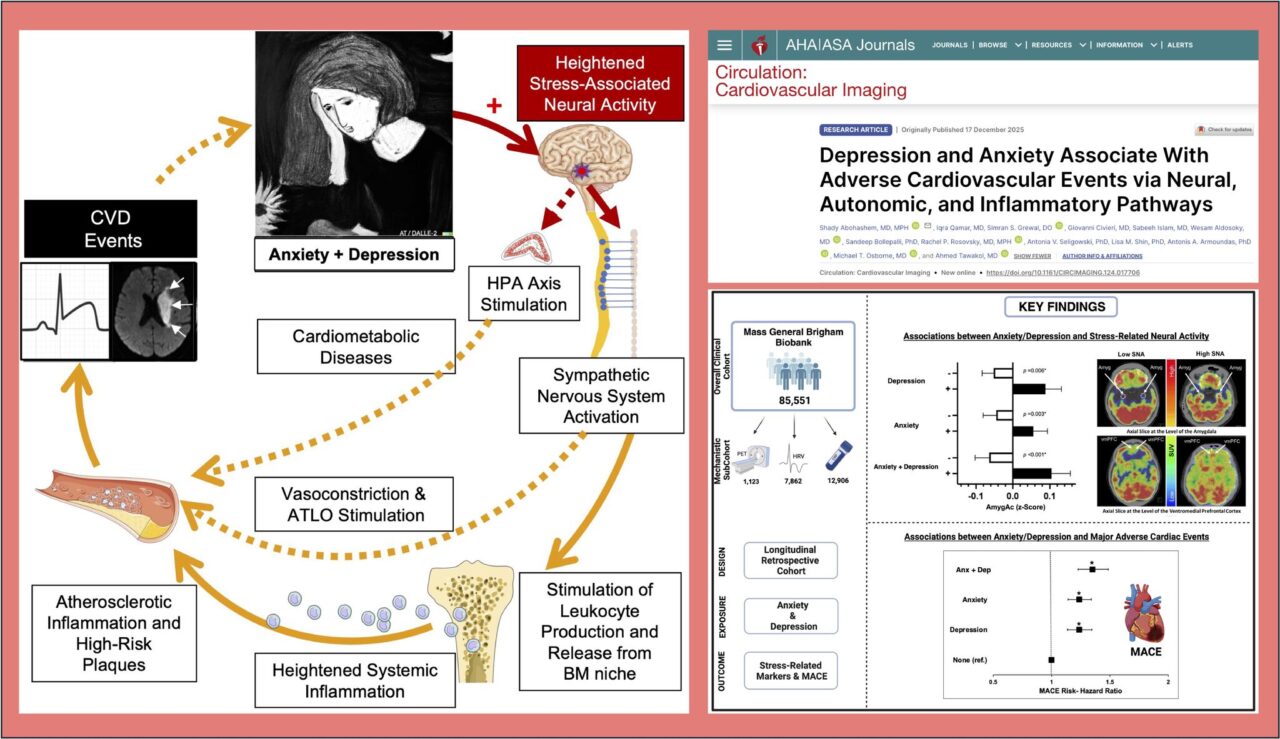
In our newly published study in Circulation: Cardiovascular Imaging, we examined this connection at scale and in depth.
We analyzed data from more than 85,000 adults enrolled in a large U.S. biobank and followed them longitudinally for major adverse cardiovascular events , including heart attack, stroke, and heart failure.
Beyond clinical diagnoses, we integrated:
• Brain imaging to assess stress-related neural activity
• Heart rhythm data to evaluate autonomic function
• Inflammatory biomarkers to capture immune activation
What we found so far:
Depression and anxiety were each independently associated with a higher risk of cardiovascular events, even after accounting for traditional risk factors, lifestyle behaviors, medications, and socioeconomic factors.
Importantly, individuals diagnosed with both depression and anxiety had the highest risk.
Why? Because these conditions appear to converge on a shared biological pathway:
• Heightened stress-related activity in the brain
• Reduced heart rate variability (a marker of autonomic imbalance)
• Elevated systemic inflammation
Together, this forms a brain–autonomic–immune axis linking mental health to cardiovascular disease.
Depression and anxiety are not rare, isolated conditions. They frequently coexist, share overlapping brain circuitry, and often represent a continuum rather than distinct disorders. When they occur together, biological stress appears amplified, translating into greater cardiovascular risk. This helps explain why addressing mental health is not simply about improving quality of life, it may also be critical for preventing heart disease.
Bottom line
– Mental health leaves biological fingerprints, and those fingerprints matter for the heart.
– Recognizing and treating depression and anxiety may be a powerful, and still underutilized, strategy for cardiovascular prevention.
Grateful to the outstanding study team and collaborators: Iqra Qamar, Simran Grewal, Giovanni Civieri, Sabeeh Islam, Wesam Aldosoky, Sandeep Bollepalli, Rachel Rosovsky, Antonia V. Seligowski, Lisa M. Shin, Antonis Armoundas, Michael T Osborne, Ahmed Tawakol.”
Stay with Hemostasis Today to discover more.
-
Feb 23, 2026, 18:13Fight4Hematology Supports Research and Empowers the Next Generation – ASH
-
Feb 23, 2026, 17:59Wolfgang Miesbach: Real-World Evidence of Emicizumab on Joint Outcomes in Hemophilia A
-
Feb 23, 2026, 17:56Shiny K Kajal: The Transfusion Reaction We Often Miss
-
Feb 23, 2026, 17:53Radheshyam Meher: Contributing to the Transfusion Evidence Round-Up for International Childhood Cancer Day 2026
-
Feb 23, 2026, 17:46Mahesan Subramaniam: The Physiological Impact of Anger on Immunity
-
Feb 23, 2026, 17:42Bryan Fry: First Evidence That Bothrops atrox Venom Directly Activates Human Factor VII
-
Feb 23, 2026, 17:34Bastu Odoka: Why Blood Should NOT be Left at the Bedside to ‘Warm’
-
Feb 23, 2026, 17:28Henry Burkitt: Patients Are Challenging How the Medicines Policy System Works in England
-
Feb 23, 2026, 16:50Mutaz Al‑Sabah: Interesting Webinar on FH in Women is Now Available to Watch

