
Dr. Rawnak Sharif Shares Clinical Case: High-Risk AF Patient with Traumatic SDH
Dr. Rawnak Sharif, Resident Medical Officer at Apollo Imperial Hospital, posted on LinkedIn:
“High-Risk AF Patient with Traumatic SDH: Strategic Anticoagulation
Case Summary:
A 69-year-old male with severe ischemic cardiomyopathy (left ventricular ejection fraction 20%, chronic total occlusion) on apixaban presented after alcohol ingestion with vomiting, headache, right ear bleeding and a fall. Imaging revealed a large left-sided subdural haematoma (SDH), intracerebral and subarachnoid haemorrhage, diffuse axonal injury and right parietal/temporal fractures. Computed tomography angiography (CTA) and computed tomography venography (CTV) showed no aneurysm or vascular lesion.
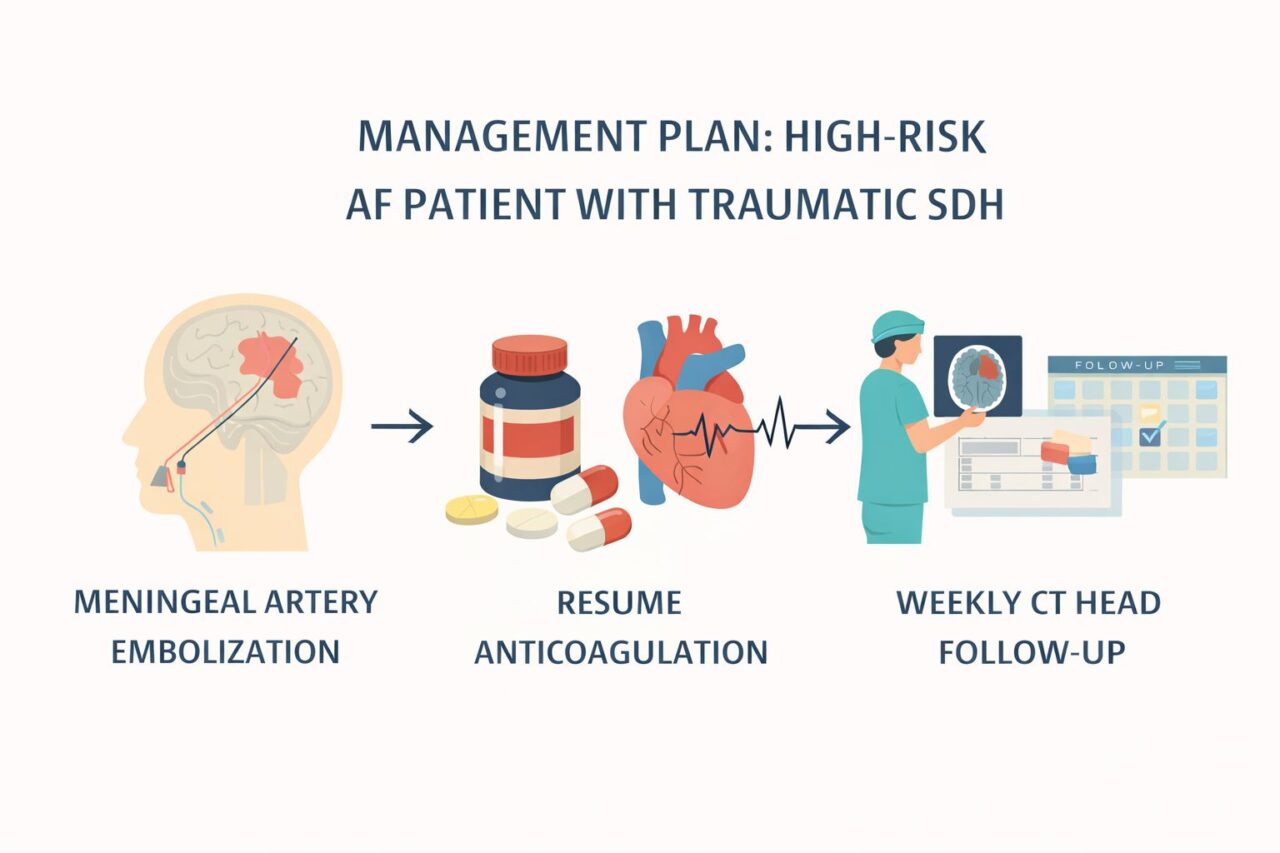
Management Plan:
- Meningeal artery embolisation (MMAE): To seal the bleeding source.
- Resumption of apixaban post-embolisation: For atrial fibrillation stroke prevention.
- Conservative neuro care: Antiedema therapy, antiepileptics, nimodipine and vitamin K.
- Weekly CT head follow-up: Until SDH stabilisation.
Clinical Summary for Practising Doctors:
- MMAE: Is increasingly validated for acute, subacute and chronic SDH. It targets the haematoma membrane’s vascular supply to reduce recurrence and promote resolution.
- Resumption of anticoagulation or antiplatelet therapy post-MMAE: Appears safe. Studies show no significant increase in SDH recurrence or haematoma size compared with withholding therapy.
- Early resumption (approximately 1 week to 1 month): May lower thromboembolic risk without increasing bleeding complications.
- Limitations: Most evidence is retrospective; patient selection bias exists. Large prospective trials are ongoing to define optimal timing and patient subsets.
Clinical Rationale:
- Traumatic SDH + AF: Requires balancing haemorrhage control with thromboembolic prevention.
- Embolisation addresses the bleeding source enabling safe anticoagulation resumption.
- Multidisciplinary decision-making (neurology, neurosurgery, cardiology) is essential.
- Structured imaging follow-up guides timing and safety.
1-Minute Bedside Checklist:
- Confirm SDH stability on repeat CT scan.
- Assess thromboembolic risk (CHA₂DS₂-VASc, devices, prior events).
- Assess bleeding risk (volume, location, comorbidities).
- Plan anticoagulation timing (post-embolisation, individually tailored).
- Choose agent (DOAC preferred if eligible).
- Multidisciplinary consultation and patient counselling.
References:
- Acta Neurochir 2025 – MMAE reduces SDH recurrence.
- PubMed 39880622 – Safe anticoagulation post-MMAE.
- PMC 10249073 – Early resumption feasible.
- Trials J 2025 – RELACS RCT, timing anticoagulation post-SDH.
Takeaway:
In high-risk atrial fibrillation patients with traumatic SDH, MMA embolisation enables safe and timely resumption of anticoagulation, reducing thromboembolic risk while minimising rebleeding. Weekly imaging and multidisciplinary care are key to optimal outcomes.”
Explore more cases for deeper insights into hemostasis with Hemostasis Today.
-
Feb 23, 2026, 18:13Fight4Hematology Supports Research and Empowers the Next Generation – ASH
-
Feb 23, 2026, 17:59Wolfgang Miesbach: Real-World Evidence of Emicizumab on Joint Outcomes in Hemophilia A
-
Feb 23, 2026, 17:56Shiny K Kajal: The Transfusion Reaction We Often Miss
-
Feb 23, 2026, 17:53Radheshyam Meher: Contributing to the Transfusion Evidence Round-Up for International Childhood Cancer Day 2026
-
Feb 23, 2026, 17:46Mahesan Subramaniam: The Physiological Impact of Anger on Immunity
-
Feb 23, 2026, 17:42Bryan Fry: First Evidence That Bothrops atrox Venom Directly Activates Human Factor VII
-
Feb 23, 2026, 17:34Bastu Odoka: Why Blood Should NOT be Left at the Bedside to ‘Warm’
-
Feb 23, 2026, 17:28Henry Burkitt: Patients Are Challenging How the Medicines Policy System Works in England
-
Feb 23, 2026, 16:50Mutaz Al‑Sabah: Interesting Webinar on FH in Women is Now Available to Watch

