
What Clinicians Should Know About ITP – Insights from Samwel Mikaye
Samwel Mikaye, CEO of SaMik Medical Center, posted on LinkedIn:
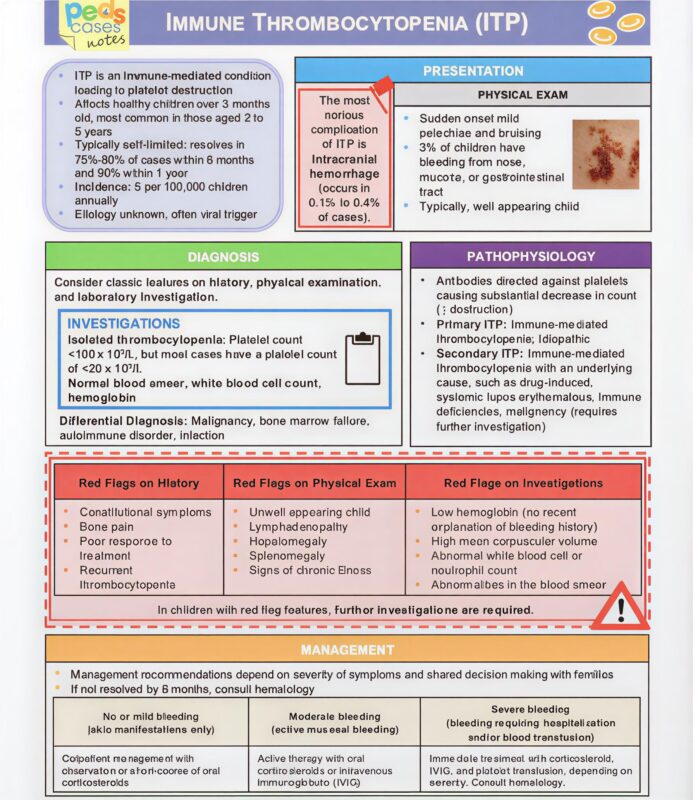
”IMMUNE THROMBOCYTOPENIC PURPURA (ITP)
Definition
Immune Thrombocytopenic Purpura (ITP) is an autoimmune disorder characterized by:
• Isolated thrombocytopenia (platelets <100,000/µL)
• Caused by autoantibodies against platelet surface antigens → accelerated destruction in the spleen and reduced platelet production in the bone marrow.
Classification
1. Primary ITP
• Idiopathic (no identifiable cause).
2. Secondary ITP
• Associated with underlying conditions:
• HIV, HCV, EBV
• Autoimmune diseases (e.g., SLE)
• Drugs (heparin, quinine, sulfa drugs)
• Vaccination (rare)
Epidemiology
• Children: usually acute, post-viral, self-limiting.
• Adults: usually chronic, more common in women <40 years.
Clinical Features
• Often asymptomatic except for bleeding.
• Mucocutaneous bleeding:
• Petechiae, purpura, ecchymoses
• Epistaxis, bleeding gums, menorrhagia
• No splenomegaly (splenic enlargement suggests another diagnosis).
Key: Patient appears well despite very low platelet count.
Diagnosis
Diagnosis of exclusion.
• CBC: isolated thrombocytopenia; other cell lines normal.
• Peripheral smear: normal red/white cells, reduced platelets.
• Coagulation profile (PT/PTT): normal
If atypical features (anemia, leukopenia, splenomegaly), consider other causes (TTP, leukemia, DIC).
Tests to rule out secondary causes:
• HIV, HCV testing
• ANA (if autoimmune disease suspected)
Management
Children (acute ITP)
• Observation if mild bleeding and platelets >30,000/µL.
• If treatment needed (significant bleeding):
• Corticosteroids (Prednisone)
• OR IVIG (for rapid platelet rise)
• Anti-D immunoglobulin (if Rh+ and not splenectomized)
Adults (chronic ITP / symptomatic)
First-line treatment:
• Corticosteroids: Prednisone or Dexamethasone pulse
• OR IVIG (if severe bleeding or need rapid rise—e.g., surgery)
Second-line options (if refractory or steroid-dependent):
• Thrombopoietin receptor agonists (TPO-RAs):
• Romiplostim, Eltrombopag
• Rituximab (anti-CD20 antibody)
• Splenectomy (curative in ~60–70% cases)
Platelet transfusion only for life-threatening bleeding; not routinely effective since autoantibodies destroy transfused platelets.
Treatment Thresholds (Adults)
• Platelets ≥ 30,000/µL + no bleeding → observe
• Platelets < 30,000/µL or active bleeding → treat
Prognosis
• Children: 80% recover spontaneously.
• Adults: chronic in ~60–70%, but manageable.”
Stay informed with Hemostasis Today.
-
Feb 27, 2026, 17:19Selma Turkovic: BTEDG Announces New Date for Wrong Blood in Tube Webinar
-
Feb 27, 2026, 17:14Mariia Kumskova: Platelet Activation and Spreading Defects in Ehlers-Danlos Syndrome
-
Feb 27, 2026, 17:11Megan Griffiths: Highlighting Pediatric PH Challenges at PVRI 2026 Congress
-
Feb 27, 2026, 17:09Gyan Barik: First-In-Human Trial for Axana Stroke Detection Is Complete
-
Feb 27, 2026, 17:05Sumedha Dash: Honored to Successfully Complete the Advanced Certificate in Transfusion Medicine
-
Feb 27, 2026, 17:02Jeff June: Building the Biological Map for Stroke Neuroprotection
-
Feb 27, 2026, 16:55Jorge Monge: Time to Implement Universal Fetal Genotyping for RhD-Negative Pregnant Women
-
Feb 27, 2026, 16:49Ana Codo: When Environmental Particles Disrupt a Fundamental Immune Function
-
Feb 27, 2026, 16:46Wolfgang Miesbach: Gut Feelings About Thrombosis – Microbiota as a Vascular Risk Factor

