
Bhanu Hima Kumar Gadamsetti: 2018 vs 2026 AHA/ASA Acute Ischemic Stroke Guidelines
Bhanu Hima Kumar Gadamsetti, Academic registrar in Neurology at Apollo Hospitals, shared a post on LinkedIn:
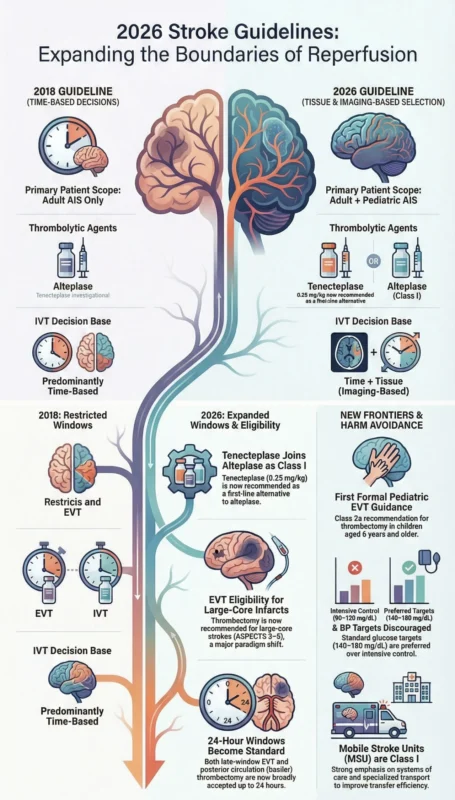
“2018 vs 2026 AHA/ASA Acute Ischemic Stroke Guidelines — What Has Truly Changed?
Over the past two years, I have consistently emphasized that tissue perfusion — not just time — is the key determinant in acute stroke management.
The 2026 guidelines now clearly reflect this shift toward imaging-based, tissue-guided decision-making, reinforcing that preserving salvageable brain tissue is central to improving outcomes in acute ischemic stroke.
1. Scope and Philosophy
2018
- Adult-focused
- Predominantly time-based decisions
- Conservative eligibility expansion
2026
- Adult and Pediatric AIS
- Imaging-based (time and tissue) selection
- Expanded reperfusion eligibility
- Strong emphasis on systems of care and harm avoidance
2. Intravenous Thrombolysis (IVT)
Thrombolytic Agent
- 2018: Alteplase only
- 2026: Tenecteplase (0.25 mg/kg) or alteplase — both Class I recommended
Tenecteplase is now first-line alternative
NIHSS and Disability
- 2018: NIHSS severity emphasized
- 2026: Any disabling deficit should receive IVT — NIHSS alone should not delay therapy
Non-disabling stroke
- 2026: IVT not recommended; DAPT preferred
Extended Window
- 2018: Mainly MRI DWI–FLAIR mismatch
- 2026: Perfusion-based IVT up to 9 hours, including wake-up/unknown onset strokes
3. Endovascular Thrombectomy (EVT)
Time Window
- 2018: 0–6 hrs standard; 6–24 hrs selective
- 2026: 0–24 hrs broadly accepted with imaging selection
Large Core Infarcts
- 2018: Mostly excluded
- 2026: ASPECTS 3–5 recommended; even 0–2 reasonable in select cases
Major paradigm shift
Posterior Circulation
- 2018: No strong recommendation
- 2026: Class I recommendation for basilar artery thrombectomy (≤24 hrs)
Pre-stroke Disability
- 2026: mRS 2 patients now included
Pediatric EVT (NEW)
- ≥6 years: Class 2a
- <6 years: Class 2b selected cases
First formal pediatric interventional guidance
4. Blood Pressure and Glucose — Evidence-Based Harm Statements
BP
- Aggressive SBP <140 mmHg discouraged
- Intensive post-EVT BP lowering harmful
- Prehospital BP lowering not beneficial
Glucose
- Intensive control (80–130 mg/dL) harmful
- Standard target remains 140–180 mg/dL
5. Stroke Systems of Care
2026 strongly emphasizes:
- Context-specific transport planning
- Door-in–Door-out (DIDO) efficiency
- Structured interhospital transfer protocols
- Mobile Stroke Units — Class I recommendation
- Neurointerventionist credentialing mandated
6. Imaging Strategy
- Early CTA strongly emphasized
- Perfusion imaging central for late-window decisions
- Pediatric preference: MRI/MRA (CT acceptable if rapid)
What Is Completely New in 2026?
- Pediatric AIS pathway
- Tenecteplase as standard thrombolytic
- Large-core EVT
- Basilar artery thrombectomy (Class I)
- Mobile Stroke Units (Class I)
- Harm-based BP and glucose statements
- Mandatory EVT quality metrics”
Stay updated with Hemostasis Today.
-
Feb 19, 2026, 14:10Gonçalo Ferraz Costa: Modern Thrombolytic Strategies and the Risk–Benefit Balance in Valve Thrombosis
-
Feb 19, 2026, 14:07Stéphanie Forté: New Insights on Stroke in Adults with Sickle Cell Disease
-
Feb 19, 2026, 14:00Hugh Kearney: Highlighting the Relevance of the Inflammasome in Multiple Sclerosis Pathophysiology
-
Feb 19, 2026, 13:56Ney Carter Borges: Low-Carbohydrate and Low-Fat Diet Quality and CHD Risk
-
Feb 19, 2026, 13:51Raul Santos: International Collaborative Insights into the Treatment of Homozygous FH
-
Feb 19, 2026, 13:38Abdul Mannan: 240 Flashcards on Acquired Underproduction Anemias
-
Feb 19, 2026, 13:36Sarah Mount: Pregnancy, Hypercoagulability, and Erythritol
-
Feb 19, 2026, 13:36Shiny K. Kajal: Cold Agglutinins Can Mimic Macrocytosis on CBC
-
Feb 19, 2026, 13:29Salihu (Oyiza) Asimawu: What If Blood Could Be Prepared in the Lab?

