
Dr Venkatesh BS: PVT Is No Longer a Contraindication for Liver Transplantation
Dr Venkatesh BS, Transplant Surgeon at CareVue Health, posted on LinkedIn:
”Establishing Portal Venous Inflow in Liver Transplant with Portal Vein Thrombosis – A Practical Surgeon’s guide
Portal vein thrombosis (PVT) is no longer a contraindication for liver transplantation. It’s a challenge that tests a surgeon’s planning, anatomy sense, and adaptability.
Our roadmap drawn from experience and evolving evidence:
1. Define and Plan
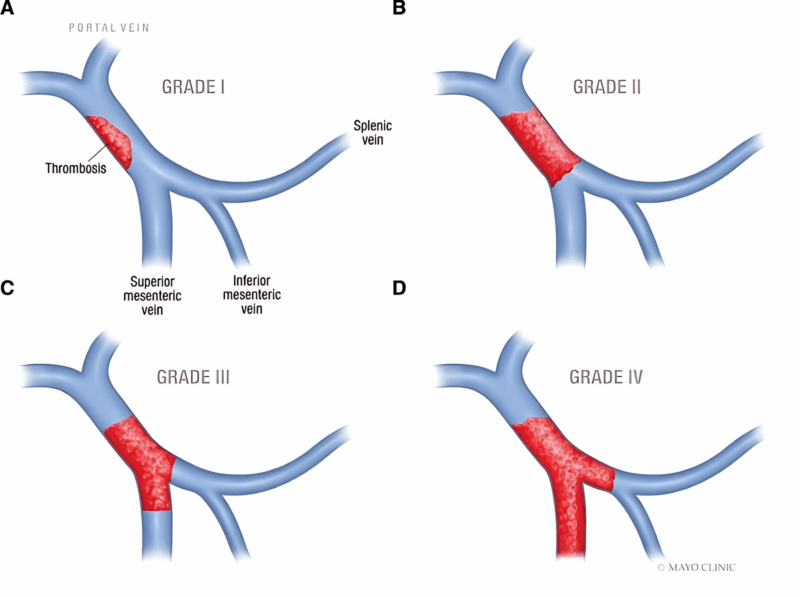
• Grade the PVT (Yerdel classification) – partial (I-II) vs complete with/without SMV involvement (III-IV).
• Map venous anatomy using CECT/MRV: assess SMV patency, cavernoma, and collaterals (especially spleno-renal shunts).
• Always have backup inflow options planned before incision.
2. Surgical Techniques for Portal Flow Reconstruction
Low-Grade (Yerdel I-II): Thrombectomy
• Eversion thrombectomy by gently peeling the thrombus off the intima.
• Confirm backflow from SMV and perform end-to-end portal anastomosis.
Intermediate (Yerdel III): Mesoportal Jump Graft
• When native PV unusable but SMV patent. sometimes a collateral can be used as inflow too.
• Conduit: donor iliac vein (preferred) or cryopreserved/autologous vein.
• Create a smooth, tension-free SMV → conduit → graft PV anastomosis.
Extensive (Yerdel IV): Alternative Inflows
• Renoportal anastomosis: for large spleno-renal shunts.
• Cavoportal hemitransposition: salvage option in diffuse splanchnic thrombosis.
• Multivisceral transplant: the definitive frontier when splanchnic venous occlusion is total, restoring full physiological portal inflow and gut drainage.
3. Intraoperative Flow Optimization
• Maintaining portal pressure <25 mmHg.
• Maintaining portal vein flow by ligating other collaterals or left renal vein in case of large shunt to augment portal flow
• Confirm flow using intraoperative Doppler before closure.
4. Surgical Pearls
• Always being prepared multiple inflow options, success often lies in the backup plan.
• Handling the SMV delicately as its our inflow lifeline.
• Early anticoagulation and Doppler surveillance are key to preventing rethrombosis.
At Madras Transplant Associates (MTA) , our philosophy has always been to adapt, innovate, and tailor reconstruction strategies to each patient’s anatomy ensuring safe and physiological restoration of portal inflow, even in the most complex PVT cases.
Multivisceral transplantation remains a fascinating frontier transforming how we approach patients with complete splanchnic thrombosis and offering renewed hope where once there was none.
How do you prefer to handle an unexpected Grade IV thrombosis? Renoportal first or straight to hemitransposition?
Let’s share experiences and technical insights- learning together helps push the boundaries of what’s possible.”
Stay updated with Hemostasis Today.
-
Jan 29, 2026, 14:02Emma Lefrancais on Alarmin IL33 and Platelet Biology
-
Jan 29, 2026, 13:44Sia A: One of My Favorite Conversations from ASH
-
Jan 29, 2026, 13:34Sarah Matuja on Tanzania Stroke Project
-
Jan 29, 2026, 13:28Nancy Di Salvo on Amplifying Rare Disease Voices Through Partnership
-
Jan 29, 2026, 13:21Raul Santos Shares The Results of ORION-16: On The Efficacy and Safety of Inclisiran
-
Jan 29, 2026, 05:22Aravind Palraj Draws a Comparison Between APS and Lupus Cerebritis
-
Jan 29, 2026, 05:09Edina Cenko on Expanding Cardiovascular Risk: From Ischaemia to Emerging Frontiers
-
Jan 29, 2026, 04:58Anna Randi Shares the Latest Episode of The VWF and Angiogenesis Story from Her Lab
-
Jan 29, 2026, 04:49Ruah Alyamany on Her Contribution to Establishing The Role of IgM in APS
