
Pulmonary Thromboembolism Explained: From Virchow’s Triad to Imaging, Treatment, and Complications
Notas De Patologia posted on X:
”Pulmonary Thromboembolism (PE)
Definition
Pulmonary thromboembolism (PE) is the partial or complete obstruction of the pulmonary arterial circulation by emboli, most often originating from deep vein thrombosis (DVT) of the lower limbs or pelvis.
PE is part of venous thromboembolic disease (VTE), which includes both DVT and PE.
Epidemiology
Estimated 8–10 million VTE cases/year worldwide.
In the United States: ~900,000 cases/year, with in-hospital mortality up to 30% if untreated.
PE is the 3rd leading cause of cardiovascular death (after myocardial infarction and stroke).
Can occur at any age, but incidence increases in the elderly.
Risk increases with hospitalization, immobilization, surgery, and cancer.
Etiology and Pathophysiology
Virchow’s Triad
Venous thrombosis formation and subsequent PE are associated with:
Venous stasis (e.g., immobilization, surgery, trauma).
Endothelial injury (e.g., catheters, trauma, surgery).
Hypercoagulability (e.g., malignancy, thrombophilia, oral contraceptives, antiphospholipid syndrome).
Pathophysiological consequences
Vascular obstruction → increased pulmonary vascular resistance → acute right ventricular overload.
Hypoxemia → due to ventilation/perfusion mismatch and intrapulmonary shunting.
Systemic inflammatory response → cytokine-mediated vasoconstriction worsens perfusion.
In massive PE → obstructive shock and acute cor pulmonale.
Clinical Manifestations
Sudden dyspnea (most common symptom).
Pleuritic chest pain.
Cough, hemoptysis (in pulmonary infarction).
Tachycardia, palpitations.
Syncope/hypotension in massive PE.
Signs of DVT in lower limbs: pain, swelling, tenderness, warmth.
Severe cases → hemodynamic instability, shock, sudden death.
Laboratory Diagnosis
D-dimer: sensitive but non-specific; useful to rule out PE in low-risk patients.
Arterial blood gases: may show hypoxemia and respiratory alkalosis (hyperventilation).
Troponin and BNP: may be elevated in massive PE (RV strain).
Imaging and Pathology Findings
Imaging
CT pulmonary angiography (gold standard): directly visualizes intraluminal thrombi.
Ventilation/perfusion (V/Q) scan: alternative when CT is contraindicated.
Transthoracic echocardiography: indirect signs (acute pulmonary hypertension, RV dilation).
Venous Doppler ultrasound: can identify associated DVT.
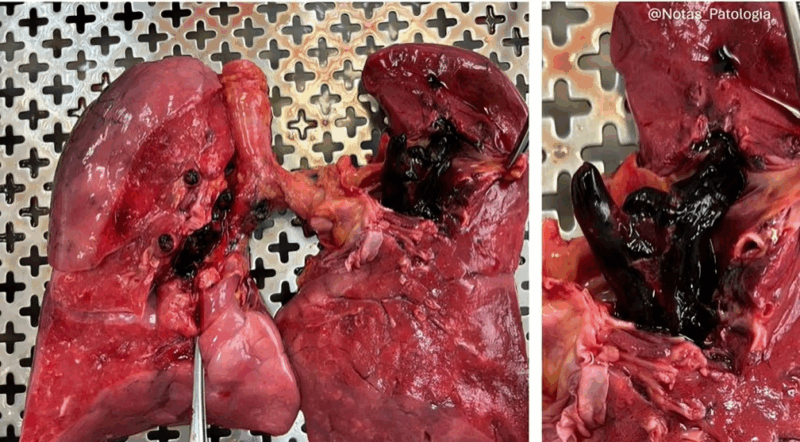
Pathology
Lungs with wedge-shaped hemorrhagic infarcts.
Intravascular thrombi, sometimes undergoing organization.
In fatal cases: massive embolus in main pulmonary arteries → acute cor pulmonale.
Differential Diagnosis
Acute myocardial infarction.
Pneumonia.
Pneumothorax.
Acute decompensated heart failure.
Severe asthma/bronchospasm.
Aortic dissection.
Prognosis and Complications
Untreated PE: mortality up to 30%.
With appropriate treatment: mortality reduced to 2–8%.
Complications:
Chronic thromboembolic pulmonary hypertension (CTEPH).
Chronic cor pulmonale.
VTE recurrence.
Treatment
Hemodynamic stabilization: oxygen therapy, cautious fluids, vasopressors if needed.
Anticoagulation (cornerstone of therapy): unfractionated heparin, low molecular weight heparin, or direct oral anticoagulants (DOACs).
Thrombolysis: indicated for massive PE with hemodynamic instability.
Surgical or catheter embolectomy: in refractory cases.
Inferior vena cava filter: for patients with absolute contraindications to anticoagulation.
Summary
Pulmonary embolism (PE) is a potentially fatal condition caused by obstruction of the pulmonary circulation, usually by thrombi from DVT.
Clinical presentation ranges from mild dyspnea to circulatory collapse and sudden death. Early diagnosis with CT pulmonary angiography and prompt initiation of anticoagulation are critical to reducing mortality.
Long-term complications, such as chronic thromboembolic pulmonary hypertension (CTEPH), should always be considered in follow-up.
Disclaimer: This content is for educational purposes only and does not replace professional medical evaluation.
References:
World Health Organization (WHO) – Venous thromboembolism: Report of a WHO Scientific Group.
Konstantinides SV, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2020;41:543–603.
PathologyOutlines.com – Pulmonary embolism.
Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379(9828):1835–1846.”
Stay updated with Hemostasis Today.
-
Jan 22, 2026, 15:36We Must Roll Up Our Sleeves And Help: José Antonio García Erce on Plasma Donation
-
Jan 22, 2026, 15:25Nita Radhakrishnan on Challenges In Congenital Afibrinogenemia
-
Jan 22, 2026, 15:10Jin Q Gives a Summary of 2025’s Most Impactful Cell and Gene Therapy Milestones
-
Jan 22, 2026, 14:57Nirav Dhanesha on CD14 Acting As A Functional Driver of DVT
-
Jan 22, 2026, 11:41Jamilla Goedegebuur and Colleagues on VTE Management in Case of PAD
-
Jan 22, 2026, 11:28Abdulrahman Katib on API-CAT Trial’s Evaluation of Apixaban Dosing
-
Jan 22, 2026, 11:19Bruno Odisio: Ablation Margins Are Software-Dependent
-
Jan 22, 2026, 10:38Pedro Perez: The VTE Market Is Clearly Entering Its Next Phase
-
Jan 22, 2026, 10:29Marvin Garcia Reyes Presents a Case of Aorto-Visceral and Aorto-Iliac Thrombosis
