
Dr Abdul Mannan on the Echinocyte: Mastering the Diagnostic Duality of Artifact vs. Pathology
Dr Abdul Mannan, Consultant Haematologist at Betsi Cadwaladr University Health Board, posted on LinkedIn:
“The Diagnostic Duality of the Echinocyte: Mastering the Artifact vs. Pathology Conundrum
Few findings are as deceptively simple—yet diagnostically complex—as the echinocyte.
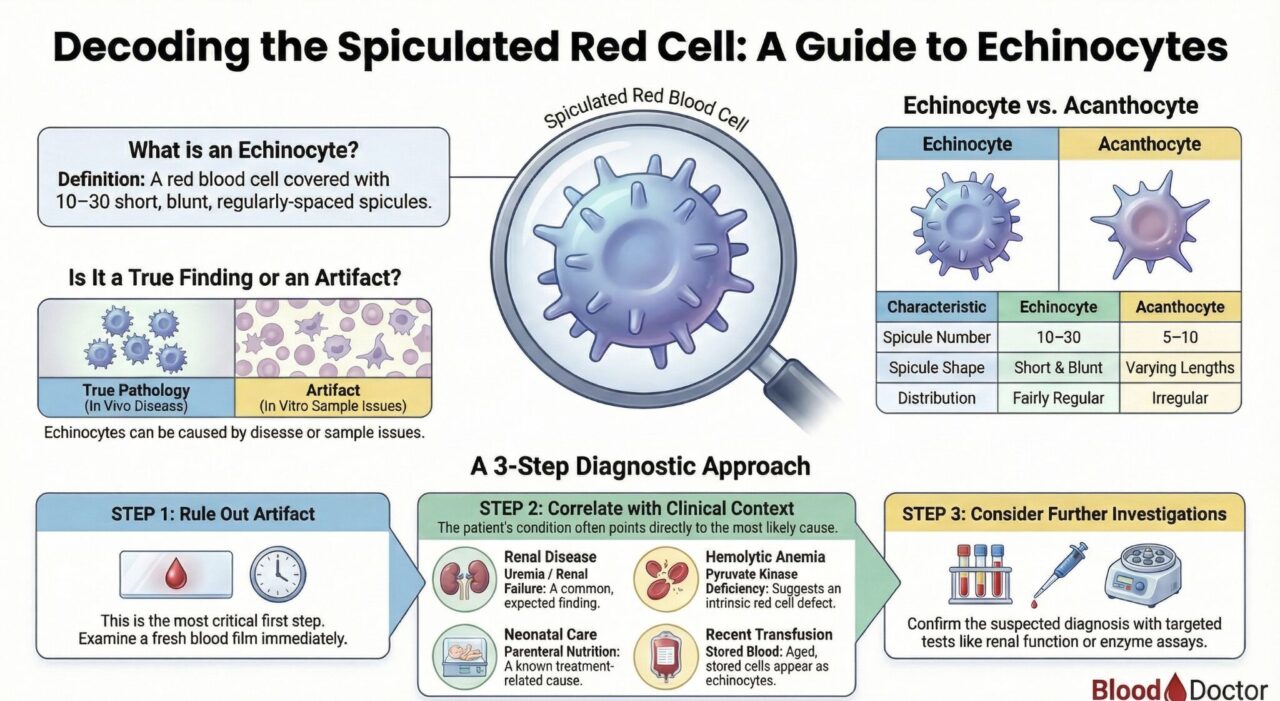
Often confused with the acanthocyte, the echinocyte is an erythrocyte defined by its 10–30 short, blunt spicules of fairly regular form.
However, the most crucial lesson in teaching echinocyte identification is not merely recognizing its shape, but understanding its diagnostic duality: Is this pathology, or is this an artifact?
An impressive hematologist knows that reporting ‘echinocytes present’ is only the beginning. The true value lies in systematically unlocking their meaning.
The Professional’s 3-Step Protocol for Echinocytes
When an automated alert or initial film suggests echinocytosis, the systematic approach immediately transforms a simple observation into a powerful diagnostic tool.
Step 1: Rule Out Artifact
The formation of echinocytes in vitro is remarkably common. Before considering systemic disease, you must exclude technical causes.
• Test for Time & Storage: Echinocytes are a common storage artifact if the blood sample (especially in EDTA) sits too long.
• Test for Contamination: Check for potential contamination (e.g., heparin), which can induce echinocyte formation.
• Confirm Persistence: Prepare a fresh wet preparation immediately. True in vivo echinocytes will persist; artifacts often disappear.
Step 2: Correlate with Clinical Context (Plasma vs. Cell Defect)
Once artifact is excluded, evaluate the clinical status against the known mechanisms:
1-Pathway Alteration of Plasma Environment (All cells affected)
Renal failure (uremia), Hyperthermia, Snake/Bee Venom
Renal failure (uremia), Hyperthermia, Snake/Bee Venom
2-Intrinsic Red Cell Abnormality (Only proportion affected)
ATP deficiency (e.g., Pyruvate Kinase deficiency)
Neonates, Patients with haemolytic anaemia
Step 3: Consider Targeted Investigations
The clinical context dictates the next action:
• If renal failure is suspected: Order Renal Function Tests
• If an enzyme defect is suspected: Order PK
• Review the history for Chlorpromazine or Parenteral Nutrition
The echinocyte is a fascinating morphological messenger. Its appearance requires us to move beyond basic pattern recognition and apply a rigorous, systematic, and clinically integrated approach. This discipline is what separates a technician from a hematology expert.”
Follow the latest with Hemostasis Today.
-
Mar 1, 2026, 13:17Michael Makris։ Extraterrestrial Regolith as a Trigger of the Intrinsic Coagulation Pathway
-
Mar 1, 2026, 13:11Strategic Planning Day to Shape The Future of Thrombosis and Haemostasis – THANZ
-
Mar 1, 2026, 13:06Simon Senanu: Not Every Thrombocytopenia Is Real
-
Mar 1, 2026, 12:53Kevin Tang: Evolving Burden of CVD Across Asia and Its Broader Implications for Global Health Policy
-
Mar 1, 2026, 12:02Hassan Raza: Building Sustainable Support for People with Bleeding Disorders in Pakistan
-
Mar 1, 2026, 11:40Naradja Wissmar: Raised IL-32 as a Hint to Long-Term Immune Activation Post-COVID
-
Mar 1, 2026, 11:10Mehran Ghasemzadeh: A Novel Panel Bridging Platelet Function and Clinical Presentation in Chronic ITP
-
Mar 1, 2026, 10:47Tagreed Alkaltham: In Transfusion Medicine, Every Reaction Deserves An Answer
-
Mar 1, 2026, 10:31Deborah Siegal Explores ARTESiA in The CLOT Conversation’s Latest Episode

